When facing gastrointestinal issues, understanding the complexities of a colon operation can empower patients to make informed decisions about their health. This surgical procedure, often required for conditions such as colorectal cancer, diverticulitis, or inflammatory bowel disease, plays a critical role in restoring digestive health. In this blog post, we will explore everything you need to know about a colon operation, from the indications for surgery to the types available and what to expect during the entire process. By breaking down each aspect, we aim to equip you with the knowledge necessary for effective preparation, recovery, and post-operative care, ultimately guiding you towards a smoother journey to better health.
What is a Colon Operation?
A colon operation, commonly referred to in the medical field as colorectal surgery, encompasses a range of surgical procedures aimed at addressing various conditions affecting the colon, which is a crucial part of the large intestine. This operation is generally performed to treat diseases, injuries, or abnormalities, offering a solution to restore normal function and improve overall health. Understanding the nuances of this surgical intervention can empower individuals to make informed decisions regarding their health.
Scope of Colon Operations
The colon is responsible for absorbing water and nutrients from undigested food, and it plays a pivotal role in forming and storing waste. When the colon becomes compromised due to a plethora of issues, a surgical procedure may be necessary. The surgeries involve various methods and techniques, allowing healthcare professionals to tailor the approach to the patient’s specific needs.
In essence, the types of procedures that can qualify as a colon operation include:
| Procedure | Description |
|---|---|
| Colostomy | Creation of an opening in the abdominal wall to divert stool into a bag outside the body. |
| Colectomy | Removal of part or all of the colon; can be total or partial, depending on the condition. |
| Polypectomy | Removal of polyps in the colon to prevent cancer development. |
| Bowel Resection | Surgical resection and reconnection of sections of the intestine affected by disease. |
| Laparoscopic Surgery | Minimally invasive approach using small incisions and a camera, leading to quicker recovery. |
Reasons for Undergoing a Colon Operation
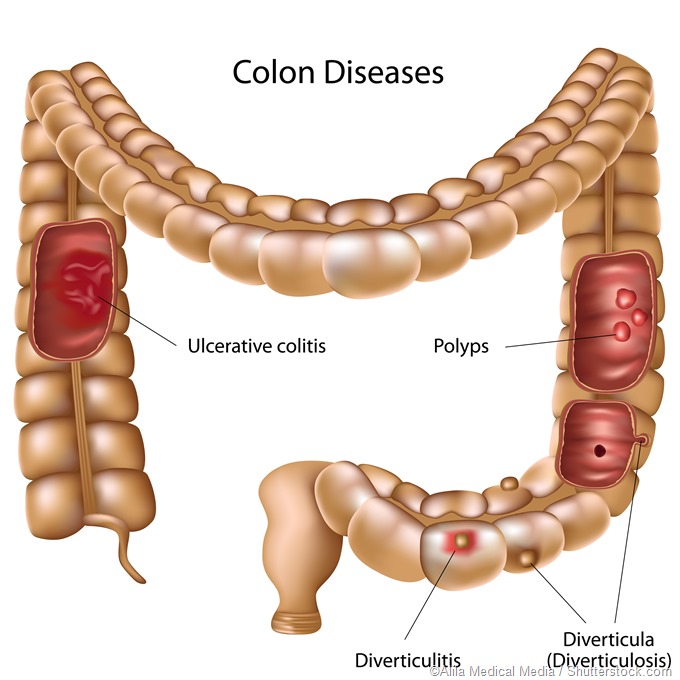
There are several reasons why healthcare providers may recommend this surgical intervention. Common indications include:
- Colorectal Cancer: Removal of cancerous sections to prevent the spread of malignancy.
- Diverticulitis: Surgical treatment for inflammation or infection of diverticula (pouches in the colon).
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease or ulcerative colitis may necessitate surgery when medication fails.
- Trauma: Injuries that damage the colon can lead to surgical interventions.
- Fecal Incontinence: When conservative measures fail, surgery may restore bowel control.
Importance of a Multidisciplinary Approach
Prior to undergoing a colon operation, patients often consult various specialists, including gastroenterologists, surgeons, and nutritionists. This multidisciplinary approach ensures comprehensive care, where the specific condition is assessed, and the appropriate surgical strategy is formulated.
Key Takeaways
Understanding the essentials of colon operations can greatly assist adults in recognizing their options and potential outcomes. By being informed about what the procedure entails, including the types of surgery and their indications, individuals can engage in a productive dialogue with their healthcare providers. This collaborative effort helps mitigate anxiety and fosters a smoother transition into preoperative and postoperative phases of care.
In summary, a colon operation not only addresses physical ailments but also plays a crucial role in enhancing quality of life for those facing such challenging health issues. By understanding its scope and significance, patients are encouraged to participate actively in their health care journey.
Indications for Undergoing a Colon Operation
Colon operations are often performed for various medical reasons, reflecting the crucial role that the colon plays in the digestive system. Understanding the specific indications for undergoing such surgical procedures can greatly assist patients in making informed decisions about their health. Below is an exploration of common indications, structured for clarity and ease of understanding.
1. Colorectal Cancer
One of the most significant reasons for a colon operation is the presence of colorectal cancer. This form of cancer can develop in either the colon or rectum and may necessitate surgical intervention to remove cancerous tumors. Early detection through screening procedures such as colonoscopies is vital, as this can lead to more effective treatment options.
2. Diverticulitis
Diverticulitis occurs when small pouches (diverticula) in the colon become inflamed or infected. For patients experiencing recurrent diverticulitis or severe complications such as abscesses, perforation, or fistulas, surgical options may be recommended. During the operation, the affected sections of the colon are typically removed, allowing for improved digestive function.
3. Inflammatory Bowel Disease (IBD)
Chronic conditions like Crohn’s disease and ulcerative colitis fall under the umbrella of inflammatory bowel disease. These conditions can lead to severe inflammation and damage to the colon. In cases where medical management proves ineffective or when complications arise, surgery may become necessary to remove affected segments of the colon.
4. Bowel Obstruction
A bowel obstruction, often caused by scar tissue, tumors, or inflammation, can impede the normal passage of waste. When patients experience acute abdominal pain, vomiting, or a significant inability to tolerate food, surgical intervention may be required. The operation can involve the removal of the obstructed section of the bowel, thereby restoring normal function.
5. Familial Adenomatous Polyposis (FAP)
Familial adenomatous polyposis is a genetic disorder characterized by the development of numerous polyps in the colon. These polyps carry a high risk of progression to colorectal cancer. In such cases, prophylactic surgery to remove the colon is often recommended to prevent cancer development.
6. Severe Constipation
For some individuals, chronic constipation can lead to fecal impaction and significant discomfort. When dietary and lifestyle modifications or medications fail to alleviate the condition, surgical options may be explored. Operations may involve removing parts of the colon to help restore normal bowel function.
Summary Table of Indications for Colon Operation
| Indication | Description |
|---|---|
| Colorectal Cancer | Removal of cancerous tumors for effective treatment |
| Diverticulitis | Surgery for inflamed diverticula causing complications |
| Inflammatory Bowel Disease | Resection of affected colon areas due to chronic conditions |
| Bowel Obstruction | Removal of parts of the bowel to relieve obstruction |
| Familial Adenomatous Polyposis | Prophylactic removal of the colon to prevent cancer |
| Severe Constipation | Resection for relief from chronic constipation and impaction |
This detailed look at the indications for colon operations provides insight into conditions that necessitate surgical intervention. These conditions underscore the importance of regular medical check-ups and consultations, which can assist in the early detection and management of potential issues. Awareness and understanding can lead to better health outcomes, as patients become active participants in their healthcare journeys.
Types of Colon Surgeries
When it comes to addressing various colorectal conditions, different types of surgeries are performed based on the specific medical needs of patients. Understanding these types can help patients feel better informed and prepared for potential treatments. Below, we outline several key types of colon surgeries, each tailored for distinct problems.
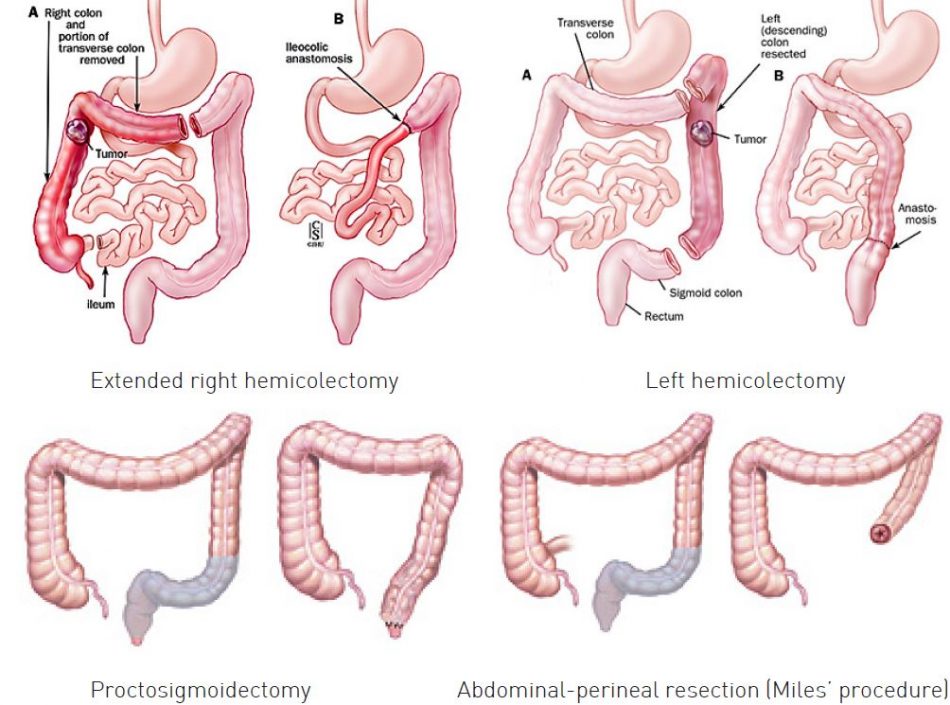
Resection
One of the most common colon surgeries is resection, where a part of the colon is surgically removed. This procedure is often performed for:
| Conditions | Details |
|---|---|
| Cancer | Tumors may require segmental or total removal to prevent metastasis. |
| Diverticulitis | Severe inflammation or infection necessitates removal of affected segments. |
| Bowel Obstruction | Blockages due to scar tissue or foreign bodies may require resection. |
Resection can involve either an open approach or laparoscopic techniques, depending on the surgeon’s judgment and the patient’s condition.
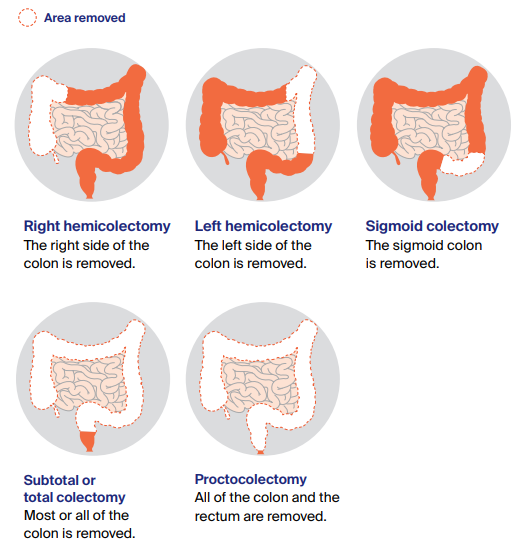
Colectomy
Colectomy is a broader term that refers to the surgical removal of the entire colon and can be classified as:
| Type | Description |
|---|---|
| Total Colectomy | Complete removal of the colon; often performed in severe cases like familial polyposis. |
| Partial Colectomy | Removal of a specific segment, which can then be reconnected to the rectum, if feasible. |
Individuals undergoing colectomy might need to adopt specific dietary changes as part of their recovery.
Colonoscopy with Polypectomy
A colonoscopy may also involve a polypectomy, where polyps (growths on the colon lining) are removed during the colon examination. This minimally invasive procedure is crucial for:
| Advantages | Details |
|---|---|
| Cancer Prevention | Removing polyps helps reduce the risk of developing colorectal cancer. |
| Symptom Relief | Removal of polyps can alleviate symptoms such as rectal bleeding or obstruction. |
This procedure generally requires minimal recovery time.
Ileostomy and Colostomy
In certain cases, particularly when there is extensive damage or disease in the colon, an ileostomy or colostomy may be necessary. Both surgeries involve creating an opening (stoma) in the abdominal wall for waste elimination, but differ in mechanics:
| Surgery Type | Description |
|---|---|
| Ileostomy | Involves the removal of the colon with the ileum (the last part of the small intestine) attached to the stoma. Waste is expelled directly into an external pouch. |
| Colostomy | Part of the colon is removed, and a stoma is created from the remaining portion of the colon. This can be temporary or permanent depending on the patient’s condition. |
Endoscopic Mucosal Resection (EMR)
EMR is an advanced technique where elevated lesions in the colon are removed endoscopically. This method allows for:
| Benefits | Details |
|---|---|
| Minimal Invasion | Reduces recovery time and complications associated with major surgery. |
| Targeted Treatment | Is effective for early-stage cancers and pre-cancerous conditions. |
Each type of colon surgery serves a specific purpose and is chosen based on a patient’s unique circumstances. Discussing options with a healthcare provider can provide greater clarity on what to expect and how best to prepare for surgery.
Preparation for a Colon Operation
Preparing for a colon operation is a critical step towards ensuring a successful surgical outcome. Understanding what is involved in the preparatory phase can help patients feel more informed and less anxious about the upcoming procedure. The preparation generally involves several key components, including dietary changes, medication management, laboratory tests, and psychological readiness.
Dietary Adjustments
In the week leading up to the colon operation, it is often recommended that patients make specific dietary changes. These modifications typically involve a low-fiber diet for a few days prior to the surgery. The purpose of this diet is to prevent the formation of stool, facilitating a cleaner surgical site.
Further dietary guidelines may include:
| Day | Dietary Recommendations |
|---|---|
| 3-4 Days Before | Start low-fiber foods (e.g., white bread, rice, eggs) |
| 1-2 Days Before | Transition to a clear liquid diet (e.g., broths, gelatin, clear juices) |
| Night Before | Fasting after midnight, following physician advice |
This gradual transition into a lighter diet often helps ease digestion and reduces the likelihood of complications during the surgery.
Medication Management
Before the surgical procedure, it is essential for patients to discuss their current medications with their healthcare provider. Some medications may need to be adjusted or temporarily halted, especially blood thinners or any medication that affects blood clotting. Patients should provide a complete list of their current medications and any over-the-counter supplements they may be taking.
It is crucial to follow specific instructions regarding medication use, as missing a dosage or improperly managing these medications can lead to increased risks during and after the operation.
Laboratory Tests and Assessments
Prior to the colon operation, healthcare providers typically recommend a selection of laboratory tests. These exams may encompass blood tests to check the patient’s overall health and determine any underlying conditions that could impact surgery. Additionally, depending on individual health status, imaging tests, such as CT scans or X-rays, might be necessary to provide a clearer view of the surgical area.
| Test Type | Purpose |
|---|---|
| Complete Blood Count (CBC) | Evaluate overall health and identify any issues, such as anemia |
| Coagulation Tests | Assess how well the blood clots, important for surgery preparation |
| Electrolyte Check | Ensure balance and function before surgery |
Psychological Readiness
It is common for patients to experience anxiety leading up to a surgical procedure. Engaging in relaxation strategies, such as deep breathing exercises, meditation, or talking with a therapist, can significantly aid in managing these feelings. Informing family and friends about the operation can also provide emotional support, as having a strong support system can ease pre-surgery jitters.
Final Preparations
On the day of the colon operation, patients will typically need to arrive at the healthcare facility early for final preparatory measures, which may include an additional health assessment and the administration of any necessary pre-operative medications. Patients should ensure they have someone available to drive them home post-operation, as the effects of anesthesia can linger for several hours.
With thorough preparation, individuals can head into their colon operation feeling empowered and ready for the journey ahead.
What to Expect During the Procedure
Undergoing a procedure involving the colon can be daunting, but understanding what to expect during the operation can simplify the experience. Specifically, various factors contribute to the overall process, including the type of anesthesia used, the surgical approach taken, and the expected duration of the procedure. Below is a detailed breakdown of each element that you can anticipate during the surgical intervention.
Pre-Operative Preparations
Before entering the operating room, you will undergo several pre-operative preparations:
- Fasting: Patients are generally required to fast for a specific duration before the surgery, usually at least 8-12 hours, to ensure an empty stomach.
- Medication Review: The healthcare team will review your medications to pinpoint any that may need to be paused or adjusted to maintain safety during the operation.
- Intravenous (IV) Line: An IV line will often be placed in your arm for administering medications, fluids, and anesthesia.
Anesthesia Administration
Most colon surgeries require anesthesia to ensure patient comfort. Key options include:
| Type of Anesthesia | Description |
|---|---|
| General Anesthesia | This involves complete unconsciousness. You won’t feel any pain and will have no awareness during the procedure. |
| Regional Anesthesia | This form numbs a specific area of the body, commonly used for localized procedures. The patient may be awake but pain-free. |
After anesthesia is administered, doctors will position you correctly on the operating table, ensuring you are comfortably situated for the duration of the surgery.
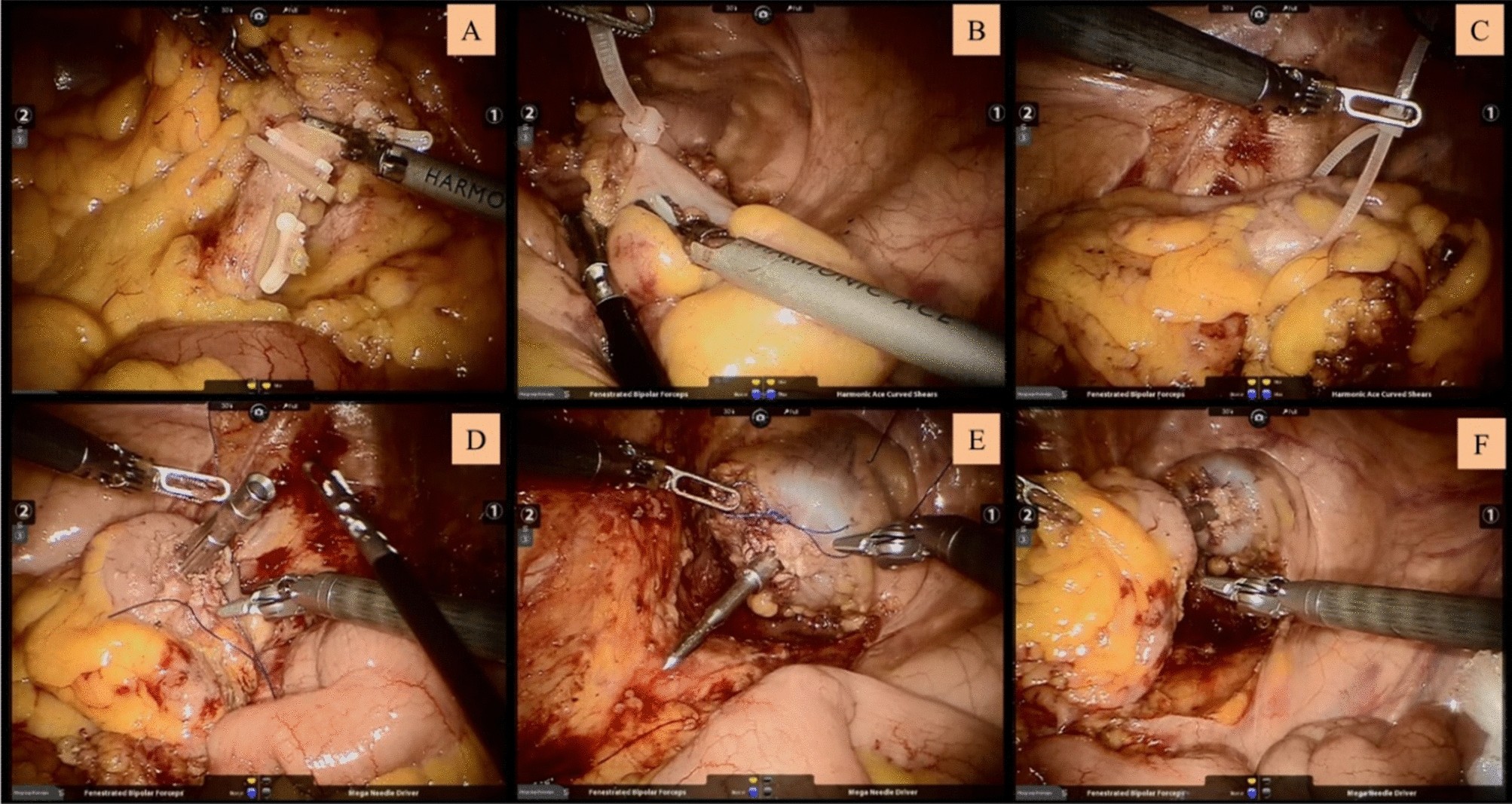
Surgical Techniques
The choice of surgical technique greatly influences what happens during the procedure. The two primary approaches are:
- Open Surgery: This traditional method requires a larger incision in the abdomen. Surgeons have direct access to the colon and surrounding organs, allowing for greater visibility but often resulting in longer recovery times.
- Laparoscopic Surgery: This minimally invasive technique involves several small incisions and the use of a camera. Surgeons can manipulate instruments through these small openings, typically leading to shorter recovery periods and less postoperative pain.
Intraoperative Monitoring
Throughout the procedure, medical staff will closely monitor vital signs, including heart rate, blood pressure, and oxygen levels. Several specialized professionals will be present, from the surgeon and surgical assistant to anesthesiologists, each playing a vital role in ensuring everything runs smoothly.
Duration of the Procedure
The overall length of the procedure varies based on multiple factors such as the type of surgery performed and individual case specifics. Typically, surgeries involving the colon may last anywhere from 1 to 4 hours.
Post-Anesthesia Transition
After the surgical component, patients will be taken to a recovery area where the effects of anesthesia are closely monitored. Here’s what to expect:
- Initial Recovery: You may feel drowsy and experience some discomfort. Nurses will monitor your vitals, including how well you’re waking up from anesthesia.
- Pain Management: Medications for pain relief are often administered at this phase to ensure a comfortable transition from the procedure.
Understanding these various elements of what happens during the procedure can alleviate anxiety and prepare you for the experience ahead. This preparation can empower you with the knowledge that while colon surgery may seem intimidating, it is a well-structured and meticulously managed process aimed at promoting your long-term health and recovery.
Recovery process after a colon operation
Recovering from a colon operation can be a significant phase in your healing journey. The recovery timeline varies depending on the type and extent of the surgery performed, your overall health, and adherence to post-operative care guidelines. Understanding what to expect can help alleviate anxiety and guide you through the initial stage of recovery.
Immediate Post-Operative Phase
Once the surgery is completed, you will be monitored closely in a recovery room. Typically, patients are observed for several hours as they awaken from anesthesia. This initial phase focuses on ensuring that vital signs stabilize, any immediate complications are addressed, and pain is effectively managed.
Key Aspects:
- Vital Signs Monitoring: Heart rate, blood pressure, and oxygen levels are monitored.
- Pain Management: Healthcare providers will assess your pain level and may provide medications via IV or orally.
- Fluid Intake: You may start with IV fluids until your healthcare team determines that your bowel function is returning.
Hospital Stay Duration
Usually, the hospital stay can range from 2 to 7 days post-surgery, depending on the complexity of the procedure and your recovery progress. During this time, certain assessments are routinely conducted. These might include:
- Assessing bowel movements and discharge.
- Checking for signs of infection or complications, such as fever or abdominal swelling.
- Monitoring nutrition status and ensuring that you can gradually progress to a regular diet.
Returning to Daily Activities
As you transition from the hospital to your home, it will be essential to allow your body ample time for healing. Generally, most individuals can resume light activities within a week or two but should avoid heavy lifting, intense exercise, or physically demanding tasks for about 4 to 6 weeks.
General Guidelines for Daily Activity:
| Activity | Expected Timeline |
|---|---|
| Light walking | Within 1-2 days |
| Returning to work (light duty) | 2-4 weeks |
| Full return to physical activities | 4-6 weeks |
Nutrition and Hydration
Post-operative nutrition plays a critical role in recovery. Initially, a liquid diet might be recommended to allow your digestive system to recover. As you tolerate liquids, fiber-rich foods can gradually be introduced to promote healthy bowel function.
Suggested Diet Plan Timeline:
- Day 1-2: Begin with clear liquids (broth, water, and gelatin).
- Day 3-4: Progress to full liquids (smoothies, puddings).
- Day 5 onward: Introduce a balanced diet, focusing on fruits, vegetables, whole grains, and lean proteins.
Monitoring Recovery Signs
During the recovery phase, close attention must be paid to your body’s signals. Report any unusual symptoms to your healthcare provider promptly, such as:
- Increased abdominal pain or swelling.
- Persistent nausea or vomiting.
- Changes in bowel habits.
- Signs of infection, like fever above 101°F or the presence of pus from incisions.
In summary, the recovery process following a colon operation involves multiple stages of healing, from immediate post-operative care in the hospital to managing home recovery, nutrition, and lifestyle adjustments. Perhaps the most crucial aspect of this journey is effective communication with your healthcare team; being proactive about your recovery can significantly enhance your healing experience.
Potential Risks and Complications
Undergoing a colon operation, like any surgical procedure, carries certain risks and potential complications. Understanding these risks is crucial for individuals contemplating the surgery. By being informed, you can partner effectively with your healthcare provider to manage these concerns proactively. Below, we outline some common risks associated with colon surgeries.
Common Risks of Colon Operations
While many patients recover well from colon surgeries, it is essential to be aware of the potential complications. The most common risks include:
| Risk | Description |
|---|---|
| Infection | Surgical site infections can occur, leading to pain, swelling, and fever. Prompt medical attention is crucial in such cases. |
| Bleeding | Significant bleeding may require blood transfusions or additional surgical procedures to address the issue. |
| Anesthesia complications | Rarely, reactions to anesthesia may occur, leading to respiratory issues or allergic reactions. Thorough pre-operative assessments can help minimize these risks. |
| Bowel obstruction | Scar tissue from the surgery can lead to blockages in the intestines, which may require further intervention. |
| Anastomotic leak | In cases where sections of the colon are connected post-surgery, leaks can occur, potentially leading to severe infection and requiring immediate medical care. |
| Delayed recovery | Some patients can experience prolonged healing times due to various factors such as age, pre-existing health conditions, or lifestyle factors. |
Understanding Serious Complications
In addition to the common risks, there are also serious complications that may arise from colon surgeries. These include:
- Sepsis: A life-threatening body reaction to infection that can occur if bacteria enter the bloodstream. Symptoms such as rapid heart rate, high fever, and confusion require urgent medical attention.
- Peritonitis: Infection or inflammation of the peritoneum, the lining of the abdomen, leading to severe abdominal pain, fever, and nausea.
- Organ injury: Accidental damage to surrounding organs, such as the bladder, urethra, or small intestine, can occur during surgery. Depending on the severity, this may necessitate additional surgical procedures.
Risk Factors to Consider
Certain factors may elevate the risks associated with colon surgeries. These include:
- Age: Older adults may face higher risks due to decreased physiological resilience and pre-existing health issues.
- Chronic health conditions: Conditions like diabetes or heart disease can complicate recovery and increase risks of infection.
- Smoking: Tobacco use is known to slow healing and increase the risk of various complications. Quitting smoking before surgery can significantly benefit recovery.
It is essential to discuss your individual risk factors with your healthcare provider. They can offer guidance on how to minimize these risks through lifestyle modifications or additional pre-operative assessments.
Pre-operative Assessment
Before the operation, a thorough pre-operative assessment is conducted to identify any underlying health issues that may complicate the procedure. This assessment may involve:
- Blood tests: To evaluate liver and kidney function, as well as blood clotting ability.
- Medical history review: To identify prior surgeries, existing medical conditions, or medication usage that may impact the surgery.
- Imaging studies: Such as X-rays, CT scans, or MRIs to visualize the colon and assess the necessity and type of surgery required.
By carefully considering and discussing these risks, both patients and healthcare providers can work together to create a robust plan for surgical success. Open communication regarding concerns can lead to more personalized care and enhanced outcomes, paving the way for a smoother surgical experience.
Post-operative Care and Lifestyle Adjustments
After any surgical intervention, including a colon operation, proper post-operative care is crucial for a smooth recovery and the prevention of complications. Adopting specific lifestyle adjustments will also promote healing, enhance comfort, and ensure a more triumphant return to daily activities. Below, we delve into comprehensive care strategies and modifications to consider after the procedure.
1. Incorporating a Balanced Diet
Following a colon operation, your digestive system will require time to heal. Nutrition plays a pivotal role in facilitating recovery. It is essential to gradually reintroduce foods to avoid overwhelming the system. Initial dietary considerations include:
| Food Type | Recommendations |
|---|---|
| Clear liquids | Broths, gelatin, and herbal teas are ideal for the first few days. |
| Low-fiber foods | Foods such as white rice, plain pasta, and bananas can help ease your digestive load. |
| Gradual fiber increase | Once cleared by your doctor, integrate whole grains, fruits, and vegetables. |
| Hydration | Maintain adequate fluid intake, aiming for at least 8-10 cups of water daily. |
2. Pain Management
Post-operative discomfort is not uncommon. However, it’s essential to manage pain effectively to remain comfortable and engaged in recovery. Follow medical advice regarding:
- Medications: Use prescribed pain relievers and over-the-counter options only as suggested.
- Non-pharmaceutical methods: Heat packs or cold compresses can alleviate discomfort both at the incision site and other painful areas.
3. Physical Activity and Mobility
While rest is vital, gentle mobility can improve circulation and prevent complications like blood clots. Start with:
- Short walks: Begin with a few minutes daily and gradually increase distance as tolerated.
- Avoiding straining: For at least six weeks, refrain from heavy lifting and high-impact activities, as these may jeopardize the healing incision.
4. Monitoring Surgical Site
Keep a vigilant eye on the surgical site for signs of infection or unwanted complications. Key aspects to observe include:
| Signs to Observe | Indications |
|---|---|
| Increased redness | May signify infection or irritation. |
| Swelling or fluid leakage | Often requires medical evaluation for potential complications. |
| Fever above 101°F | Seek immediate medical attention. |
| Persistent pain | Might indicate issues requiring prompt care. |
5. Emotional Well-being
Post-operative recovery can affect not just the body but also mental health. Consider implementing:
- Mindfulness techniques: Practices like meditation and yoga can help reduce stress.
- Support systems: Engage with friends and family for emotional support or consider professional counseling if feelings of anxiety or depression become prominent.
6. Follow-up Care
Regular follow-up appointments are vital for monitoring recovery. During these visits:
- Discuss any concerns or symptoms.
- Ensure that you are healing well and that any adjustments in post-operative care are made as necessary.
By adhering to these care tips and lifestyle adjustments, recovery following a colon operation can be more efficient and comfortable. Each step taken promotes healing, supports physical well-being, and enables a return to an active, fulfilling lifestyle.
Follow-up Appointments and Monitoring
After undergoing a colon operation, maintaining a diligent follow-up schedule is crucial for ensuring a smooth recovery. Follow-up appointments typically entail a series of evaluations focused on assessing the surgical site, monitoring recovery progress, and promptly addressing any complications that may arise. The intervals and nature of these appointments can vary based on the complexity of the surgery and individual health circumstances.
Importance of Follow-Up Appointments
Follow-up consultations serve several key purposes:
- Wound Inspection: Healthcare professionals will assess the surgical site for any signs of infection, proper healing, or other complications that may necessitate intervention.
- Symptom Monitoring: Practitioners will inquire about any symptoms such as pain, swelling, changes in bowel habits, or signs of complications, helping to identify issues early.
- Assessment of Functionality: Follow-ups allow for the evaluation of digestive function and overall gastrointestinal health post-surgery, ensuring that the body is adapting to any changes made during the operation.
Typical Follow-Up Timeline
Understanding what to expect regarding the timing of follow-ups can alleviate anxiety for many patients. Below is a general guideline:
| Time Frame | Follow-Up Focus | Typical Tests/Examinations |
|---|---|---|
| 1-2 weeks | Initial Healing | Visual exam of the surgical site |
| 4-6 weeks | Functionality Assessment | Imaging studies if indicated, symptom review |
| 3-6 months | Long-term Recovery and Functionality | Comprehensive evaluations, lab tests |
It is essential to adhere to scheduled appointments and communicate any concerns between visits. This proactive approach can drastically improve outcomes and quality of life after surgery.
Monitoring Symptoms and Lifestyle Changes
Patients are encouraged to monitor their symptoms diligently. Keeping track of their recovery progress by maintaining a detailed diary can be helpful. This diary should include:
- Dietary changes
- Bowel movement patterns
- Any new symptoms experienced
- Pain levels and medication use
Sharing this information during follow-ups enhances the clinician’s ability to address individual concerns and adjust post-operative care as necessary.
Collaboration with Healthcare Provider
Engaging in discussions with healthcare providers during follow-up appointments is critical. Patients should feel comfortable asking questions regarding their recovery, diet, medications, or any lifestyle modifications that might be beneficial. Maintaining open lines of communication can foster a comprehensive understanding of the recovery process, paving the way for better health outcomes.
Long-Lasting Health Monitoring
In some cases, especially if individuals underwent extensive colorectal surgery or have pre-existing conditions, longer-term monitoring may be necessary. This could involve:
- Regular screening for colon cancer, especially for individuals with a history of polyps or other risk factors.
- Ongoing assessments for gastrointestinal function or any complications stemming from the surgery.
By establishing a robust follow-up schedule and committing to ongoing monitoring, patients can significantly enhance their recovery journey and promote lasting health stability.
When to Contact Your Healthcare Provider
After undergoing a surgical procedure related to the colon, staying vigilant about your health and recovery is essential. Recognizing when to reach out to your healthcare provider can make a significant difference in your recovery outcomes. Here, we will outline the critical signs and situations that warrant immediate contact with your healthcare team, ensuring you can address any complications promptly.
Signs of Potential Complications
Understanding the indicators of complications can help you to take prompt action and potentially avoid severe issues. Here is a table highlighting key symptoms to monitor closely:
| Symptom | What It May Indicate |
|---|---|
| Severe abdominal pain | Possible infection, obstruction, or perforation |
| Persistent fever (higher than 101°F / 38.3°C) | Indicates possible infection |
| Uncontrolled vomiting | May suggest blockage or complication impacting digestion |
| Unusual swelling or redness near the incision site | Could be a sign of infection or hematoma |
| Significant changes in bowel habits (diarrhea or constipation) | May indicate complications like anastomotic leak or ileus |
| Blood in stool or rectal bleeding | Could indicate hemorrhage or damage to the bowel |
| Shortness of breath or chest pain | May suggest a serious cardiovascular issue or pulmonary embolism |
Timing for Contact
It is advisable to have a list of defined triggers prompting communication with your healthcare provider. Over the first few weeks following the procedure, your sensitivities are heightened. Here are specific guidelines for when to contact your provider:
- Immediately Upon Noticing Symptoms: Symptoms such as excessive pain, fever, or bleeding should prompt an immediate call or visit to your healthcare provider.
- Inconsistent Recovery Progress: If you notice that your recovery seems to stagnate or deteriorate despite following medical advice, do not hesitate to reach out.
- Post-Operative Day 5 Attentiveness: While some discomfort and changes are normal, if symptoms worsen around day 5 post-surgery, especially abdominal pain or digestive issues, you should consult your provider.
- Any New Symptoms: If you experience unexpected changes in your health status, like sudden fatigue or lack of energy, these could be signs of an underlying issue.
Additional Recommendations
- Keep Important Numbers Ready: Have your surgical team’s contact information readily available. It can be helpful to have a list of emergency services if needed.
- Follow-Up Appointment Notices: Ensure you attend all scheduled follow-up appointments, where your healthcare provider will monitor your recovery closely.
- Education on Medication: If you notice adverse effects from prescribed pain medications or antibiotics, let your provider know, as they may need to adjust your treatment plan.
- Support Network: Inform family or friends about your condition and recovery process. They can assist you in monitoring your health and facilitating communication with medical providers when necessary.
Staying proactive and aware of your health condition while recovering from colon surgery is paramount. Understanding these triggers and following through with communication ensures that you receive timely intervention and provides peace of mind during your recovery journey. This vigilance can considerably enhance your healing process and overall health outcomes.
Frequently Asked Questions
What is a colon operation and why is it performed?
A colon operation, also known as a colectomy, is a surgical procedure to remove all or part of the colon (large intestine). This operation is primarily performed to treat various medical conditions, such as colorectal cancer, inflammatory bowel disease (IBD), diverticulitis, or bowel obstruction. By removing the affected portion of the colon, the procedure aims to relieve symptoms, prevent complications, and improve the patient’s quality of life.
What are the different types of colon operations?
There are several types of colon operations depending on the condition being treated. The main types include partial colectomy, where only a segment of the colon is removed; total colectomy, which involves the removal of the entire colon; and colostomy, where an opening is created in the abdominal wall to divert stool. The choice of procedure is influenced by the underlying disease, its location, and the overall health of the patient.
What can I expect during the recovery process after a colon operation?
Recovery from a colon operation varies by individual and the specific procedure performed. Generally, patients can expect to stay in the hospital for several days. Initial recovery may involve managing pain, adjusting to a modified diet, and gradually increasing activity levels. Full recovery typically takes several weeks, during which patients are advised to follow their surgeon’s guidelines, attend follow-up appointments, and watch for any signs of complications, such as infection or bowel obstruction.
What are the risks and complications associated with a colon operation?
As with any surgical procedure, a colon operation carries certain risks. Potential complications include infection, bleeding, blood clots, and adverse reactions to anesthesia. Additionally, there can be specific risks like leakage from the surgical site, bowel obstruction, and changes in bowel habits post-surgery. It is essential for patients to discuss these risks with their healthcare provider beforehand to make informed decisions about their treatment.
How will a colon operation affect my diet post-surgery?
Post-surgery, patients may need to adopt a special diet to aid recovery. Initially, a clear liquid diet is usually recommended, gradually transitioning to solid foods as tolerated. Patients are often advised to avoid high-fiber foods in the early stages to prevent discomfort, and should focus on balanced meals that include protein, healthy fats, and hydrated foods. Long-term dietary changes may be necessary depending on the extent of the surgery and individual health needs, typically guided by a dietitian.