Colostomy surgery can be a life-changing procedure, often necessary for individuals dealing with severe gastrointestinal issues or injuries. Understanding what this entails is crucial for anyone facing the prospect of a colostomy operation. In this comprehensive guide, we will explore the various types of colostomy procedures, how to prepare effectively for surgery, and what to expect during and after the operation. Moreover, we will provide essential tips for managing your recovery, including dietary recommendations and emotional support strategies. By equipping yourself with the right information, you can navigate the challenges of recovery with confidence and ensure a smoother adjustment to life post-surgery.
Types of Colostomy Procedures
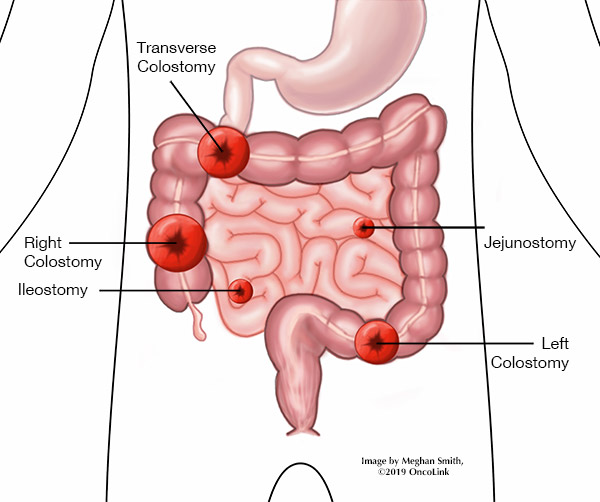
Colostomy procedures have evolved significantly over the years, leading to a variety of surgical techniques that cater to specific medical conditions, needs, and patient circumstances. Understanding the different types of colostomies is essential for patients and caregivers, as it directly influences recovery and management strategies. Below, we’ll explore the main categories of colostomy procedures, distinguishing features, and their intended purposes:
Primary Types of Colostomies
| Type of Colostomy | Description | Indications |
|---|---|---|
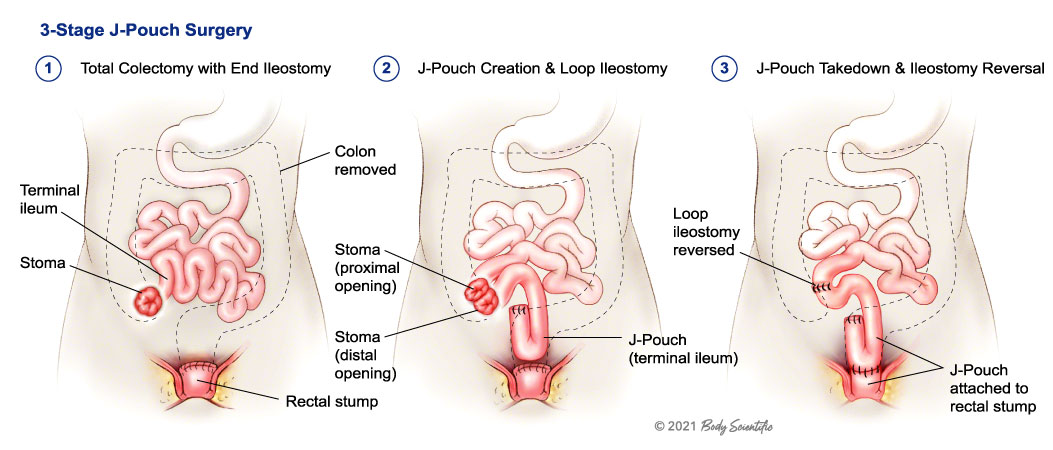
| Temporary Colostomy | A reversible procedure where a portion of the colon is bypassed. | Typically performed after surgical interventions for conditions like trauma, diverticulitis, or bowel obstruction. |
| Permanent Colostomy | A long-term solution where part of the colon is removed. | Often necessary due to colorectal cancer or severe bowel diseases. |
Colostomy Designs
While the two primary types above define the overarching categories of colostomy procedures, various surgical designs further refine each type. These designs address different parts of the colon and allow for tailored solutions based on individual needs.
- Ascending Colostomy:
- Description: Involves bringing the ascending colon to the abdominal wall.
- Use Case: This type of colostomy is less common and primarily recommended for individuals with diseases affecting the lower intestine.
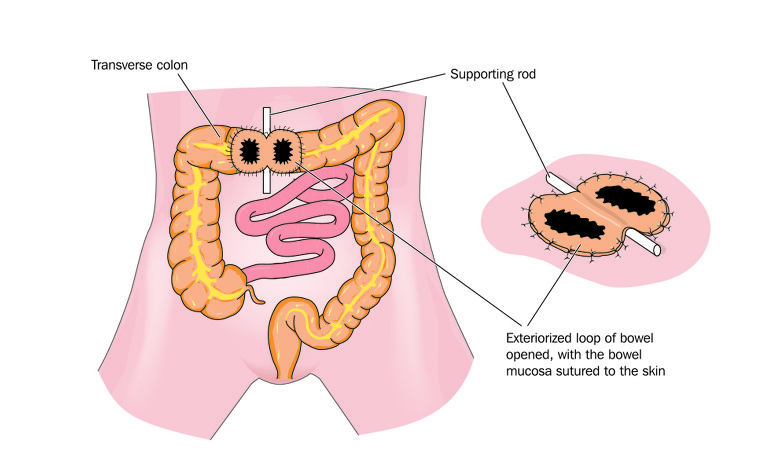
- Transverse Colostomy:
- Description: Here, the transverse colon is brought out through a horizontal incision on the abdominal wall.
- Use Case: It serves as a temporary measure, often used during emergency interventions or to allow healing processes post-surgery.
- Descending Colostomy:
- Description: The descending colon is brought to the surface, typically producing more solid stool.
- Use Case: Commonly performed in patients who may have lost sections of the colon or require ongoing bowel management.
- Sigmoid Colostomy:
- Description: This involves the lower part of the colon and is the most frequently performed type.
- Use Case: It aids those who have conditions such as diverticulitis or malignancies, providing a pathway for stool elimination.
Factors Influencing Colostomy Selection
Choosing the appropriate type of colostomy involves several considerations, which can include:
- Underlying Medical Conditions: The reason for the colostomy, like cancer or bowel obstruction, significantly affects the type selected.
- Surgeon’s Recommendation: Surgeons will evaluate and recommend the best possible procedure based on the individual’s anatomy and health status.
- Patient Lifestyle: Understanding a patient’s daily life and activities influences the colostomy design, aiming for the greatest quality of life post-surgery.
It’s paramount for patients to have open discussions with their healthcare providers regarding the best possible approach suited to their unique situation. Each type of colostomy serves a distinct purpose and has unique aftercare considerations, paving the way for better adaptation and recovery in the long run. As each individual’s needs and situations vary widely, informed decisions in collaboration with medical professionals are crucial to optimize outcomes.
Preparing for Colostomy Surgery
Preparing for a colostomy surgery can seem daunting, but taking the right steps can significantly ease anxiety and facilitate a smoother surgical experience. This process involves emotional, physical, and logistical preparations that are essential not only for optimal outcomes but also for patient peace of mind. In this section, we will outline key elements of preparation, strategies to alleviate concerns, and practical steps to streamline the surgical experience.
Understanding Pre-Operative Instructions
Before surgery, medical professionals provide detailed pre-operative instructions that patients should carefully follow. This information typically includes:
| Instruction | Details |
|---|---|
| NPO Guidelines | Patients may be required to abstain from food and drink for a specific period leading up to the operation. Typically, this means remaining “nothing by mouth” (NPO) starting the night before the procedure. |
| Medication Adjustments | Patients need to inform their doctor about all medications they are taking. Some drugs, particularly blood thinners and certain supplements, may need to be adjusted or temporarily stopped to minimize surgical risks. |
| Health Assessments | A pre-surgery assessment, including physical exams and possibly lab tests (blood work, imaging), will be necessary to evaluate overall health status. |
Attending Educational Sessions
Many healthcare facilities offer educational sessions designed to prepare individuals for colostomy surgery. These sessions cover what to expect before, during, and after the operation. Attending these sessions can help demystify the procedure and clarify any lingering doubts or apprehensions. In addition, patients can ask questions about:
- Surgical techniques and their implications.
- The expected recovery timeline and challenges.
- Lifestyle changes post-surgery.
Preparing Your Home Environment
Creating a supportive environment at home can greatly influence recovery. Considerations may include:
- Organizing Your Space: Arrange frequently used items within easy reach. Ensure your kitchen, bathroom, and living areas are accessible and equipped with necessary supplies like ostomy bags, skin barriers, and wipes.
- Establishing a Healing Space: Designate a tranquil spot in your home for rest and recovery. Add comfort elements, such as pillows, soft blankets, and entertainment options like books or streaming services.
Emotional and Mental Preparation
Mental readiness can positively impact recovery. Here are several strategies to manage anxiety and stress:
- Journaling: Documenting thoughts and feelings can help process emotions surrounding the surgery.
- Mindfulness Techniques: Practices like deep breathing, meditation, or yoga can assist in reducing anxiety and promoting a state of calm.
- Support Network: Leaning on friends, family, or support groups can provide encouragement and a sense of belonging. Discussing fears with loved ones will help alleviate feelings of isolation.
Gathering Supplies
Prior to surgery, it’s prudent to gather essential supplies that will be required post-operation. Assemble:
- Ostomy Products: Purchase a variety of ostomy bags, skin barriers, and accessories. Consult with healthcare providers for recommendations tailored to individual needs.
- Comfort Items: These may include soft clothing, pillows for abdominal support, and easy-to-prepare meals for the initial recovery phase.
Final Thoughts
Proper preparation for colostomy surgery is a multifaceted process that blends medical, emotional, and logistical considerations. By understanding pre-operative instructions, engaging in educational opportunities, creating a conducive home environment, managing emotional health, and gathering necessary supplies, patients can navigate their surgical journey with greater confidence and ease. Remember, communication with healthcare providers is vital throughout this process, ensuring you are equipped with the knowledge and resources needed for a successful transition into recovery.
Post-Operative Care: Immediate Steps
After undergoing a colostomy operation, the immediate post-operative care is crucial for ensuring a smooth recovery process. Patients often experience a mix of emotions and physical changes following the surgery, which makes effective care essential in this critical phase. Here is a comprehensive guide to the immediate steps you should take post-surgery.
Initial Recovery in the Hospital
Following the colostomy operation, patients typically remain in the hospital for a few days to monitor their condition. During this time, healthcare professionals will focus on several key areas:
| Focus Area | Description |
|---|---|
| Vital Signs | Regular checks of blood pressure, heart rate, and temperature to detect any anomalies. |
| Pain Management | Administration of pain relief medications to ensure comfort during recovery. |
| Fluid Balance | Monitoring and managing fluid intake and output to prevent dehydration or complications. |
Wound Care
Proper wound care is vital to prevent infections and promote healing. Patients should adhere to the following guidelines:
- Keep the Area Clean: Gently wash the area around the stoma with mild soap and water, and pat it dry with a clean towel.
- Check for Signs of Infection: Look for redness, swelling, or discharge around the surgical site, which could indicate an infection. Report any concerns to the healthcare team promptly.
- Dressing Changes: Follow the healthcare provider’s instructions regarding when and how to change the surgical dressings.
Managing Bowel Function
Patients might experience altered bowel function immediately after the surgery. It is important to be mindful of:
- Initial Output: The first bowel movements post-surgery could be limited; this is normal as the bowel needs time to adjust.
- Stoma Monitoring: Check the stoma for any abnormalities, such as a change in color (it should be pinkish) or excessive swelling.
Emotional Support
Undergoing a colostomy operation can be emotionally taxing. Patients may feel anxious or worried about adjusting to life with a stoma. It’s vital to:
- Communicate Feelings: Discussing feelings and concerns with healthcare providers, family, or support groups can significantly aid emotional healing.
- Engage with Support Networks: Connecting with others who have undergone similar experiences can provide insight and reassurance.
Nutrition and Hydration
Nutritional needs post-surgery should be assessed and managed carefully. Following the operation:
- Gradual Dietary Changes: Start with clear liquids and gradually introduce solid foods as tolerated. This approach helps in understanding how the digestive system is reacting.
- Hydration is Key: Drink plenty of fluids to stay hydrated, as increased fluid loss can occur through the stoma.
Follow-Up Appointments
Planning for follow-up care is vital for ongoing recovery. Here are key points to consider:
- Schedule: Arrange follow-up visits with the surgeon or a specialized stoma nurse to address any concerns and maintain continual assessment.
- Education: Attend educational sessions regarding colostomy care and management to remain informed.
Summary of Immediate Post-Operative Steps
It’s essential to keep a checklist of immediate post-operative care actions to ensure no step is overlooked. Here’s a succinct compilation:
| Post-Operative Action | Description |
|---|---|
| Monitor Vital Signs | Regular checks for anomalies. |
| Manage Pain | Adequate medication for comfort. |
| Care for Surgical Wound | Keep clean and check for infection. |
| Observe Stoma Function | Monitor output and stoma condition. |
| Provide Emotional Support | Engage in conversations and support groups. |
| Focus on Nutrition | Gradual reintroduction of food and hydration. |
| Attend Follow-Up Appointments | Maintain communication with healthcare teams. |
Effective post-operative care, combined with emotional and psychological support, is vital in the immediate aftermath of a colostomy operation. By following these steps, patients can set the stage for a smoother recovery while adjusting to necessary changes in their lifestyle.
Managing Colostomy Output and Hygiene
Caring for a colostomy involves understanding the output from the stoma, which can vary significantly based on diet, hydration, and overall health. Maintaining hygiene around the stoma site is crucial for preventing skin irritation, infections, and ensuring comfort during daily activities.
Understanding Colostomy Output
Colostomy output primarily consists of waste material that has been diverted from the normal digestive tract. The consistency, color, and frequency of this output may differ based on the location of the colostomy and the individual’s diet. Here’s a basic overview of what to expect:
| Type of Colostomy | Output Characteristics |
|---|---|
| Ascending | Liquid, frequent, and can be very acidic |
| Transverse | Semi-liquid to thick, less frequent |
| Descending | More formed, typically thicker |
| Sigmoid | Very formed, much like typical feces |
This table helps visualize how different colostomy locations may affect output. Depending on these factors, colostomy patients may need to adapt their management techniques.
Tools for Managing Output
It is essential for individuals with a colostomy to use the appropriate tools for effective output management. The following items are helpful:
- Colostomy Bags: Variants exist, such as one-piece or two-piece systems. The choice often depends on personal comfort and output type.
- Skin Barriers: These protect the skin around the stoma from irritation caused by output leakage.
- Deodorants: Specially formulated products can help neutralize odor associated with output.
- Absorbent Pads: These can be useful as an additional layer of protection, particularly for those still in the initial stages of recovery.
Maintaining Hygiene
The skin surrounding the stoma requires regular attention to ensure that it remains clean and free from irritation. Key practices include:
- Daily Cleaning: Use mild soap and warm water to gently clean the stoma and surrounding skin. Avoid harsh soaps and alcohol-based products that can cause dryness.
- Drying Carefully: After washing, carefully pat the area dry with a clean towel. Avoid rubbing, which can cause irritation.
- Regular Inspection: Check the stoma and surrounding skin daily for any signs of redness, swelling, or irritation. Early intervention can help prevent complications.
- Changing the Colostomy Bag: Ideally, patients should aim to change their colostomy bags every 3 to 4 days, but it can be more frequent depending on individual output and activity levels. Always follow the manufacturer’s guidelines and adapt based on personal experience.
- Using the Right Size: Ensure that the colostomy bag and accessories fit snugly around the stoma without applying pressure. An ill-fitting bag can lead to leakage and subsequent skin irritation.
Tips for Comfort and Confidence
Living with a colostomy often requires a mental adjustment. Here are some tips to maintain comfort and boost confidence:
- Dietary Adjustments: Certain foods may thicken or loosen output. Keeping a food diary can help identify what works best.
- Stay Hydrated: Adequate hydration is key to managing output consistency.
- Engage in Support Groups: Sharing experiences with others can provide emotional support and practical advice.
By effectively managing output and maintaining hygiene, individuals can enhance their quality of life and ease the transition to living with a colostomy. Implementing these strategies can lead to more comfortable daily living post-surgery.
Nutrition and Diet Recommendations After Colostomy
After undergoing a colostomy, it’s essential to focus on nutritional strategies to support healing and maintain optimal health. The transition into a new dietary routine is crucial, as the digestive system may function differently post-surgery. Adhering to specific guidelines can promote comfort, enhance energy levels, and help avoid complications such as blockage or diarrhea. An individualized approach is often the best, but here are general recommendations to consider:
Initial Dietary Guidelines
1. Start Slow and Gradual
Following surgery, patients are typically advised to begin with clear liquids and gradually reintroduce solid foods. This allows the digestive system to adjust without overwhelming it.
2. Keep Hydrated
Maintaining adequate hydration is key. Aim for at least eight 8-ounce glasses of water daily. Clear fluids such as broth, gelatin, and clear juices are also good initial options.
Foods to Embrace After Surgery
Incorporating specific foods into the diet can help ease the adjustment period:
| Food Group | Recommended Foods | Benefits |
|---|---|---|
| Low-Fiber Foods | White rice, bananas, applesauce | Easy to digest; helps prevent blockages |
| Proteins | Eggs, fish, lean meats, tofu | Essential for healing and muscle repair |
| Dairy Products | Yogurt, cottage cheese (if tolerated) | Provides calcium and aids in digestion |
| Cooked Vegetables | Carrots, spinach, zucchini (well-cooked) | Nutrients support recovery without adding bulk |
| Fruits | Canned or cooked fruits without skins | Soft, easily digestible options |
Foods to Approach with Caution
As the body adjusts, there may be certain foods that should be minimized or avoided initially:
- High-Fiber Foods: Beans, whole grains, and raw vegetables can be hard to digest and may cause blockages.
- Foods That Cause Gas: Carbonated drinks, onions, broccoli, and cabbage can cause discomfort.
- Spicy Foods: Spices can irritate the digestive system and should be limited until tolerance is established.
Long-Term Nutrition Considerations
As recovery progresses, individuals can gradually reintroduce various foods. Emphasize the following long-term dietary strategies:
- Balanced Diet: Focus on a mix of carbohydrates, proteins, and healthy fats to support overall health.
- Regular Meal Patterns: Eating smaller, more frequent meals can help decrease stress on the digestive system and improve nutrient absorption.
- Monitor Dietary Tolerance: Pay attention to how the body responds to different foods to identify and avoid any triggers.
Key Nutritional Components
- Fiber: While it is important to gradually include fiber to aid digestion, initial intake should be limited. Once comfortable, incorporate soluble fiber such as oats, apples, and chia seeds.
- Vitamins and Minerals: Ensure adequate intake of vitamins A, C, K, and B vitamins to support various bodily functions. Supplementation may be necessary, and consulting a healthcare provider is advisable.
Customized Guidance and Support
Always consult with a registered dietitian who specializes in post-colostomy care. They can provide personalized dietary plans tailored to specific health needs, addressing any concerns related to output consistency or nutritional deficiencies.
Adapting to a new diet post-colostomy involves patience and experimentation. By following these nutrition and diet recommendations, individuals can significantly improve their post-operative quality of life and support long-term health.
Long-Term Adjustments to Life with a Colostomy
Adjusting to life with a colostomy can be a significant transition, requiring individuals to modify various aspects of their daily routines. Whether the colostomy is temporary or permanent, embracing these changes can foster a better quality of life. Below, we explore several vital adjustments that can help individuals navigate this new chapter effectively.
Emotional and Psychological Adaptations
One of the most critical factors for those living with a colostomy is addressing the emotional and psychological impacts. Feelings of anxiety, sadness, or embarrassment are common, especially in the initial phases post-surgery. Several strategies can mitigate these feelings:
- Counseling: Seeking professional help from a psychologist or counselor can provide a safe space to express feelings and learn coping strategies.
- Support Groups: Connecting with others who have similar experiences can alleviate feelings of isolation and provide valuable insights into handling everyday challenges.
Lifestyle Modifications
Adapting one’s lifestyle is essential for comfortably managing day-to-day activities post-colostomy. Key areas to address include:
| Area of Life | Adjustment Suggestions |
|---|---|
| Physical Activity | Start with gentle exercises like walking and gradually increase intensity. Avoid high-impact sports initially. Always consult a healthcare provider before starting a new exercise regimen. |
| Travel Plans | Plan ahead by carrying extra supplies, familiarizing oneself with accessible restrooms, and ensuring accommodations can meet specific needs. |
| Intimate Relationships | Open communication with partners regarding concerns and comfort levels can foster intimacy and reduce anxiety about physical changes. Discussing feelings can strengthen relationships. |
Dietary Changes
Dietary adjustments significantly impact the lifestyle of those living with a colostomy. It is essential to focus on a balanced diet that minimizes digestive issues. Key recommendations include:
- Gradual Introduction of Foods: After surgery, individuals should gradually introduce new foods to monitor their effects on output and digestion.
- Hydration: Increased fluid intake is crucial, especially since alterations in bowel function can lead to dehydration.
- Fiber Management: Balancing fiber intake is essential; both too little and too much fiber can cause complications. Slowly incorporating fiber-rich foods can help find the right balance.
Managing Daily Routine
Integrating daily routines with colostomy management requires an individual approach. Consider the following:
- Routine: Establish a daily schedule that includes time for changing the colostomy pouch, ensuring this aspect of personal care is integrated smoothly into everyday life.
- Clothing Choices: Opt for loose-fitting clothing that provides comfort while accommodating filtering and pouching systems. Specially designed garments for colostomy patients can offer both comfort and confidence.
Long-Term Support
Establishing a long-term support network is vital for ongoing encouragement and guidance. Resources such as:
- Ostomy Nurses: Professionals who specialize in caring for patients with a colostomy play a critical role in patient education and support.
- Online Communities and Resources: Websites and forums dedicated to colostomy care can serve as valuable tools for sharing experiences, tips, and resources.
Conclusion
Adapting to life with a colostomy doesn’t happen overnight; it requires patience, understanding, and support. However, with the right strategies and resources, individuals can thrive and regain control over their lives. Embracing these changes opens the door to a fulfilling lifestyle, proving that with the right mindset and support, a colostomy can be a part of a new beginning rather than an end.
Resources and Support for Colostomy Patients
Navigating life after undergoing colostomy procedures can be challenging, but numerous resources and support systems are in place to help patients adjust. These resources offer essential information, emotional backing, and practical assistance, enabling individuals to lead fulfilling lives post-surgery.
Types of Support Available
Different types of resources are available for those living with a colostomy, ranging from educational materials to peer support groups. Here is a comprehensive overview:
| Resource Type | Description |
|---|---|
| Patient Guides | Detailed handbooks that explain what to expect before and after surgery. |
| Webinars and Workshops | Online and in-person sessions that provide information on colostomy management. |
| Support Groups | Peer-led meet-ups offering emotional support and practical advice from peers. |
| Hotlines | 24/7 helplines for immediate questions regarding colostomy care. |
| Online Forums | Community platforms for sharing experiences and tips with other patients. |
| Healthcare Professionals | Access to specialized nurses or dietitians who can provide tailored advice. |
| Educational Videos | Instructional videos covering various aspects of colostomy care. |
Finding Support and Information
1. Healthcare Providers:
Consulting healthcare providers is a critical step in understanding the necessary lifestyle adjustments and managing colostomy care. Surgeons, stoma care nurses, and dietitians can provide personalized strategies to cope with the new changes, ensuring a smoother transition.
2. Support Groups:
Support communities, whether in-person or online, can be incredibly beneficial. They allow individuals to share experiences and learn from one another. Many organizations, such as the United Ostomy Associations of America (UOAA), offer local and national support groups, creating an atmosphere conducive to open discussion and emotional healing.
3. Educational Resources:
Numerous websites and organizations provide extensive educational material. Here are a few notable examples:
- UOAA: Offers a wealth of resources, articles, and tips specifically for colostomy patients.
- Colostomy Association: Provides downloadable guides, videos, and articles that cover the basics and advanced topics related to living with a colostomy.
4. Specialty Hotlines:
Many organizations run hotlines that provide immediate support for patients facing urgent questions or emotional distress. The UOAA has established a helpline in which trained volunteers offer encouragement and direction.
Emotional and Psychological Support
Navigating the psychological aspects of adapting to life with a colostomy can be equally crucial.
- Therapists and Counselors: Mental health professionals who specialize in coping strategies and patient recovery can assist individuals in overcoming feelings of anxiety, depression, or embarrassment that may arise.
- Peer Mentoring Programs: Engaging with someone who has been through similar experiences can significantly impact emotional well-being. These programs pair newly operated individuals with others who have successfully adapted, offering guidance and encouragement.
Frequently Asked Questions (FAQs)
Patients can often have many questions regarding lifestyle changes post-operation. Common queries might include:
- What about intimacy?: Support groups often discuss the impact of colostomy on relationships and ways to maintain intimacy.
- How to choose the right products?: Recommendations from peers and stoma care nurses can guide product selection for efficiency and comfort.
In summary, countless resources are available for colostomy patients, focused on enhancing knowledge, emotional support, and quality of life post-surgery. Each individual should explore these options, tailoring their support network to their unique needs and preferences, thereby fostering a healthier and more assured transition into everyday life.
Frequently Asked Questions
What is a colostomy operation?
A colostomy operation involves creating an opening in the abdominal wall to facilitate waste removal from the body when the normal bowel route is not an option. This procedure usually stems from various medical conditions, such as colon cancer, diverticulitis, or traumatic injury. During the surgery, a portion of the colon is brought out through the abdominal wall, forming a stoma that connects to a colostomy bag for waste collection.
What should I expect during the recovery process after a colostomy?
Recovery from colostomy surgery can vary, but generally, patients can expect to stay in the hospital for a few days post-operation. Initially, there may be pain and discomfort, which can be managed with prescribed medications. It’s vital to follow a specific diet as you heal, starting with clear liquids and gradually introducing more solid foods. Additionally, learning how to care for the stoma and colostomy bag is crucial in this period, as well as attending follow-up appointments.
How can I manage my lifestyle after a colostomy?
Post-colostomy, many individuals can return to a normal lifestyle, although some adjustments may be necessary. It’s important to learn how to care for the stoma and manage the colostomy bag effectively. Engaging in low-impact exercise can help maintain your physical health, while avoiding heavy lifting for a specified period is recommended. Also, staying informed about dietary modifications and participating in support groups can greatly enhance your overall quality of life during this transition.
Are there any dietary restrictions after a colostomy?
Yes, after a colostomy, there are some dietary restrictions that may need to be observed, particularly in the early recovery phase. Foods that are high in fiber may need to be limited initially to avoid blockages and excessive gas. Gradually, many patients can incorporate a varied diet, identifying any problem foods that may affect digestion or stoma output. Keeping a food diary can assist in tracking and managing one’s dietary intake effectively.
Can I participate in physical activities after a colostomy?
Absolutely! Most people can engage in physical activities after they have sufficiently healed from colostomy surgery. Activities like walking, swimming, and light exercise are often encouraged to promote recovery. However, high-impact sports or heavy lifting should be avoided for a certain period as advised by physicians. It’s also very beneficial to consult with a healthcare provider to receive personalized recommendations based on individual recovery progress.