In today’s world, the impact of facial trauma extends beyond physical injuries, often affecting emotional well-being and self-esteem. Facial reconstruction surgery emerges as a vital solution, offering individuals the chance to restore both appearance and function after devastating incidents. Whether due to accidents, medical conditions, or congenital issues, the need for this advanced surgical intervention has become increasingly prominent. As we explore the various aspects of facial reconstruction, from understanding the procedures involved to the essential role of a supportive multidisciplinary team, we will uncover how these transformative surgeries not only heal the physical scars but also contribute significantly to psychological recovery. Join us on this journey as we delve into the intricacies of facial reconstruction and discover the remarkable stories of resilience and hope that exemplify the power of modern medicine.
Understanding Facial Reconstruction Surgery
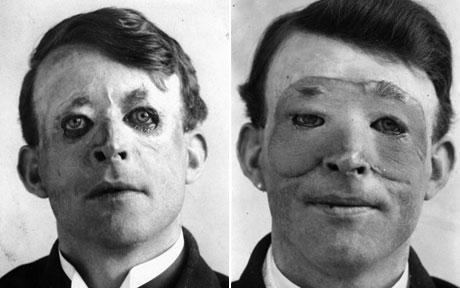
Facial reconstruction is a complex and multifaceted medical procedure, aimed at restoring the physical appearance and functional integrity of the face. This innovative practice combines surgical skills with artistic sensibility, allowing surgeons to redefine facial structures compromised by trauma, congenital deformities, tumors, or severe infections. It is important to understand that the objectives of this medical discipline extend beyond mere aesthetic enhancement; they encompass the restoration of functionality, improvement of psychological wellbeing, and overall quality of life for individuals.
Types of Facial Concerns Addressed Facial reconstruction can address a variety of conditions, each requiring specific approaches. Below is a table summarizing some common causes necessitating this type of surgical intervention:
| Cause | Description |
|---|---|
| Trauma | Injuries from accidents or violence can disfigure the facial region. |
| Congenital Defects | Conditions like cleft lip and palate present at birth require reconstruction. |
| Tumors | Removal of cancerous and non-cancerous growths may lead to significant tissue loss. |
| Infections | Severe facial infections can lead to deformities or functional impairments. |
| Aging | Natural aging processes can alter facial features, prompting rejuvenation. |
The Importance of Precision
The intricacy of the human face demands precision; every millimeter counts. Surgeons utilize advanced techniques and technologies, such as 3D imaging and computer-assisted modeling, to achieve optimal results. This level of precision not only enhances aesthetic outcomes but also aids in the restoration of functional capabilities. Various techniques, depending on the particular case, may involve tissue grafting, bone reconstruction, or even the use of implants, and each method contributes differently to the healing process.
Emotional and Psychological Considerations
The impact of facial trauma can extend deeply into an individual’s emotional and psychological health. Individuals may experience a loss of self-esteem or struggle with social interactions due to their altered appearance. Therefore, the process can also involve psychological assessments and therapeutic support to address these aspects. Surgeons and mental health professionals often work together to provide a holistic approach, ensuring that individuals are not just treated physically but emotionally as well.
The Role of a Specialist
Facial reconstruction is predominantly handled by specialized surgeons known as maxillofacial surgeons or plastic surgeons who possess advanced training in this domain. These professionals work diligently to ensure that all aspects—surgical, physical, and emotional—are effectively managed. Building a competent surgical team is vital as it involves collaboration with anesthesiologists, nurses, and rehabilitation therapists, all contributing to a more seamless recovery experience for the patient.
In summary, understanding the multifaceted nature of facial reconstruction surgeries is crucial for anyone considering or supporting someone through the process. This medical intervention not only restores harmony to the face after trauma but also plays a significant role in improving the overall well-being and psychological health of individuals affected by facial disfigurements. Through expertise, compassion, and advanced medical techniques, practitioners strive to transform lives and facilitate healing in efforts that go beyond physical restoration.

The Need for Facial Reconstruction: Causes and Conditions
Facial reconstruction surgery is often necessitated by various causes and conditions that lead to the alteration or damage of facial structures. Understanding these underlying reasons is crucial, as they define the need for such complex surgical interventions aimed at restoring both form and function. The following describes some common causes where facial reconstruction surgery becomes critical:
| Causes | Description |
|---|---|
| Trauma | Accidents, falls, or violent incidents can result in fractures and soft tissue injuries in the facial area. These traumatic events often lead to significant physical disfigurement, necessitating surgical intervention. |
| Congenital Conditions | Some individuals are born with facial deformities, such as cleft lip and palate, which may require surgical correction to improve aesthetics and function. |
| Tumors and Cancers | The removal of malignant or benign tumors in facial structures can result in gaps or deformities. Reconstructive surgery is then essential to restore the face’s integrity and functionality. |
| Infections | Severe infections, like osteomyelitis or cellulitis, can damage facial structures. This condition often demands surgical attention to remove infected tissue and reconstruct damaged areas. |
| Medical Procedures | Certain interventions, such as radical surgeries to treat cancer, can lead to significant changes in the facial structure, requiring reconstruction to restore the patient’s appearance and self-esteem. |
| Burn Injuries | Severe burns can drastically alter the appearance of an individual’s face. Reconstructive surgery aims to restore not only the outer appearance but also functionality, including the ability to speak, eat, and express emotions. |
Trauma: A Major Factor
Trauma is perhaps the most common reason for facial reconstruction surgery. Incidents such as car accidents, sports injuries, and acts of violence can lead to complex fractures and soft tissue loss. The emotional and psychological impact can be profound, as an individual’s social and personal interactions are often tied deeply to facial aesthetics.
Congenital Conditions: Birth Defects
Congenital conditions, such as cleft lips or facial asymmetries, emerge before birth and can have lasting effects on a person’s life. These conditions not only affect appearance but can also lead to difficulties in eating, speaking, and breathing. Surgical intervention is often performed in early childhood to remedy this, allowing for improved quality of life as the child grows.
Neoplastic Conditions: Cancer as a Trigger
Cancerous growths in the facial region pose a dual problem: removing the malignancy to ensure the patient’s health while minimizing physical disfigurement. Reconstruction following tumor excision is often necessary to help patients regain their confidence and restore normal function.
Infections and Burns: Complex Reconstructive Needs
In the case of infections, timely management is vital. The goal is to remove necrotic or infected tissue and then rebuild the affected area. Similarly, severe burn injuries can require multiple surgical procedures to achieve a functional and aesthetically pleasing result.
Facial reconstruction surgery, therefore, embodies a blend of medical expertise and artistry, addressing both physical impairments and the psychological toll of facial deformities. The need for these procedures arises from a clear desire to restore not just the physical attributes of an individual, but also their sense of identity and belonging, which is often profoundly affected following trauma. Each case presents unique challenges and solutions, highlighting the importance of tailored approaches to reconstruction.
The Surgical Techniques Used in Facial Reconstruction
Facial reconstruction surgery is a complex field that employs a variety of advanced surgical techniques to restore not only the physical appearance of a patient but also to restore function and improve quality of life. Each case of facial trauma or deformity presents unique challenges, thus demanding a tailored approach to surgical treatment. The techniques used in this intricate process can be broadly classified into several categories:
1. Soft Tissue Techniques
Soft tissue repair is crucial for addressing injuries that involve the skin, muscular structures, and connective tissues. Techniques employed in soft tissue reconstruction may include:
- Skin Grafting: A procedure where healthy skin is taken from another part of the patient’s body (donor site) and grafted onto the injured area to promote healing and restore appearance.
- Flap Surgery: This technique involves moving a portion of tissue along with its blood vessels to the damaged area. Flaps can be local (taken from nearby tissue) or free (taken from a distant site) and may include skin, muscle, and fat.
- Sutures and Stitching: Precision stitching techniques are critical for closing up incisions while preserving function and aesthetics.
| Technique | Description | Pros | Cons |
|---|---|---|---|
| Skin Grafting | Transferring skin from another area | Quick recovery | Possible scarring |
| Flap Surgery | Moving tissue with its blood supply intact | Enhanced vascularization | More complex surgery |
| Sutures | Closing wounds or incisions with stitches | Supports healing | Scarring may occur |
2. Bone Reconstruction Techniques
When facial bones are fractured or malformed, surgeons employ various techniques to restore structural integrity:
- Osteotomy: A procedure that involves cutting and re-aligning facial bones to achieve desired positioning. This technique is particularly useful for correcting misaligned fractures or congenital deformities.
- Bone Grafting: Similar to soft tissue grafting, this involves using bone from the patient (autograft) or a donor (allograft) to rebuild and reshape the facial structure.
- Implants: In cases where bones are significantly missing or need reshaping, surgeons may use biocompatible materials to form dental or craniofacial implants.
| Technique | Description | Pros | Cons |
|---|---|---|---|
| Osteotomy | Cutting and realigning bones | Restores function and esthetics | Invasive, longer recovery |
| Bone Grafting | Rebuilding bone structure | Natural integration | Risk of rejection |
| Implants | Using artificial materials for reconstruction | Immediate results | Risk of infection |
3. Minimally Invasive Techniques
With technological advancements, many surgeons now opt for minimally invasive approaches that reduce recovery time and complication risk:
- Endoscopic Surgery: This technique utilizes small incisions and a camera to guide the surgery, ensuring precision. It’s commonly used for addressing soft tissue injuries with minimal scarring.
- Robotic-Assisted Surgery: Surgeons can perform intricate procedures with the assistance of robotic systems, offering enhanced precision and control, which is particularly beneficial in delicate areas of the face.
| Technique | Description | Pros | Cons |
|---|---|---|---|
| Endoscopic Surgery | Minimally invasive soft tissue repair | Reduced scarring | Limited to specific cases |
| Robotic-Assisted Surgery | Advanced technology for intricate facial procedures | Higher precision | Requires specialized training |
Conclusion of the Techniques
In summary, the surgical techniques used in facial reconstruction surgery are diverse and evolve continually with technological advancements. Each technique serves a unique purpose, depending on the nature and extent of facial trauma or deformity. By understanding and utilizing these methodologies, surgeons can significantly enhance both the aesthetic and functional aspects of facial restoration, ultimately leading to improved patient outcomes and satisfaction.
The Role of a Multidisciplinary Team in Recovery
Facial reconstruction surgery is a significant step toward restoring both physical appearance and emotional well-being for individuals who have suffered trauma, congenital abnormalities, or other facial deformities. However, the journey toward recovery is seldom a solitary one; it involves a coordinated effort from a multidisciplinary team of healthcare professionals. This team typically comprises surgeons, nurses, physical therapists, psychologists, social workers, and other specialists. Each member plays a pivotal role in ensuring comprehensive care, enhancing the healing process, and optimizing outcomes.
Components of the Multidisciplinary Team
| Team Member | Role and Responsibilities |
|---|---|
| Plastic Surgeon | Responsible for performing the facial reconstruction surgery, crafting a tailored surgical approach based on individual needs and conditions. |
| Anesthesiologist | Ensures patient safety and comfort during surgery by managing anesthesia and post-operative pain control. |
| Nurses | Provide pre-operative education and post-operative care, monitor vital signs, and manage wound care and complications. |
| Physical Therapist | Assists in the restoration of facial movements and functions, using specialized exercises and therapies to enhance rehabilitation. |
| Psychologist | Offers emotional support and counseling to help patients cope with the psychological impacts of trauma and the changes that follow surgical interventions. |
| Social Worker | Helps in navigating logistical challenges, including hospital admissions and discharge planning, while providing resources for emotional and financial support. |
Collaborative Care for Enhanced Recovery
The synergy among these professionals is crucial for a successful recovery process. Collaborative care begins at the onset of treatment, where team members assess each patient’s unique needs, preferences, and medical backgrounds. Together, they design an individualized care plan that addresses every aspect of recovery—physical, emotional, and social.
For example, prior to surgery, the plastic surgeon and anesthesiologist work closely to evaluate the patient’s health status, ensuring they are well-prepared for the procedure. Concurrently, nurses educate patients about what to expect before and after surgery, which reduces anxiety and enhances cooperation.
Post-Operative Support and Rehabilitation
After surgery, the physical therapist plays a crucial role in helping patients regain functionality. They employ specific techniques to improve facial mobility, enhance muscular coordination, and promote overall recovery. This aspect of care not only focuses on the physical recovery but also addresses psychological needs, as re-establishing pre-trauma facial function significantly boosts patients’ morale.
Psychologists are integral in providing the emotional support necessary throughout the recovery phase. Trauma-related psychological responses, such as anxiety, depression, and post-traumatic stress disorder (PTSD), are common among patients who have undergone facial reconstruction surgery. A psychologist can implement strategies and therapies designed to foster resilience and coping skills.
Comprehensive Communication
Effective communication is the backbone of a successful multidisciplinary approach. Regular team meetings ensure that all members are on the same page, facilitating updates on patient progress, discussing concerns, monitoring surgical outcomes, and refining treatment protocols as needed. By ensuring a seamless flow of information, the team fosters a supportive network for the patient, leading to improved satisfaction and outcomes.
The establishment of a multidisciplinary team enhances the recovery process, increasing the likelihood that patients not only achieve physical restoration but also undergo a holistic healing journey that addresses their unique challenges. With a supportive network of diverse healthcare professionals, patients are empowered throughout their recovery from facial trauma, ensuring a comprehensive pathway to renewed confidence and improved quality of life.
Preparing for Facial Reconstruction Surgery
Preparing for any surgical procedure demands careful planning and consideration, particularly when it involves adjustments to physical appearance following trauma. Proper preparation not only promotes a successful procedure but also aids in recovery. The process can be broken down into several crucial steps to ensure that patients are mentally, emotionally, and physically ready for the journey ahead.
1. Consultation with Specialists
The first step in preparing for surgery involves an extensive consultation with various healthcare providers. This typically includes:
| Specialist | Role |
|---|---|
| Plastic Surgeon | Discuss surgical options and expected outcomes. |
| Anesthesiologist | Evaluate medical history and discuss anesthesia options. |
| Psychologist/Counselor | Address emotional and psychological readiness. |
| Nutritionist | Provide dietary recommendations that may aid in recovery. |
Each specialist plays a pivotal role in facilitating a comprehensive understanding of what to expect, thereby alleviating any fears or concerns.
2. Preoperative Assessments
Medical assessments are essential before surgery. These may include laboratory tests, imaging studies, and a physical examination. The primary objectives of these evaluations are to ensure that the patient is healthy enough to undergo surgery and to identify any potential complications. Common tests that may be performed include:
- Blood tests to assess overall health and detect any underlying conditions.
- CT or MRI scans to provide detailed images of facial structures.
- Cardiovascular evaluations if there are concerns regarding heart health.
3. Lifestyle Modifications
In preparation for surgery, patients are encouraged to adhere to certain lifestyle changes. These modifications may involve:
- Quitting smoking: Tobacco use can impair healing and increase the risk of complications.
- Avoiding alcohol: Alcohol can interfere with medications and anesthesia, potentially leading to adverse effects.
- Improving nutrition: A balanced diet rich in vitamins and minerals can bolster the immune system and enhance healing.
4. Emotional Preparation
Emotional readiness is as significant as physical preparedness. Many patients experience anxiety or distress about the surgery and its aftermath. Engaging with a mental health professional can provide strategies to cope with these feelings. Support groups or discussions with individuals who have undergone similar procedures can also offer encouragement and insights.
Psychological readiness focuses on understanding the potential changes in appearance and fostering a positive mindset toward recovery. This can create a more resilient state for managing the challenges that may arise post-surgery.
5. Arranging Postoperative Support
Planning for support during recovery is critical. Patients often require assistance as they navigate the early days following the procedure when discomfort may be prevalent, and mobility may be restricted. It’s prudent to:
- Enlist a caregiver: Family members or friends willing to assist with daily activities, medication management, and emotional support will be invaluable.
- Prepare a comfortable recovery space: Organizing a designated area with essentials within reach can create a more manageable recovery environment.
6. Understanding Post-Surgery Expectations
Educating oneself about the postoperative process is integral. Patients should familiarize themselves with expected outcomes, healing timelines, and signs of potential complications. This knowledge can lead to a sense of control and preparedness for the journey ahead.
Overall, thorough preparation is essential for optimizing the outcomes of the procedure and ensuring a smoother recovery process. By addressing physical, emotional, and logistical aspects, patients can significantly enhance their readiness for this transformative journey.
The Recovery Process: What to Expect
Recovering from facial reconstruction surgery is a crucial phase that significantly impacts the overall success of the procedure. The journey to healing involves several stages, each bringing unique challenges and milestones that can vary based on individual circumstances and the extent of the surgery.
Immediate Post-Operative Period
Once the surgery is complete, patients are typically monitored in a recovery area. During this time, you may experience swelling, bruising, and discomfort. It is essential to have a responsible adult accompany you to ensure a smooth transition home. Here’s a breakdown of what to expect immediately after surgery:
| Aspect | Description |
|---|---|
| Duration | 1-3 hours in recovery, depending on procedure |
| Monitoring | Vital signs will be checked regularly |
| Pain Management | Medication will be provided |
| Swelling/Bruising | Common and can peak around 48 hours |
First Few Days at Home
After the initial recovery period, you will return home, where continued monitoring and self-care come into play. Facial reconstruction surgery is often intense; hence adequate rest is fundamental. Within the first week, you may experience:
- Increased Swelling: This can last several days and is typically worse at night. Keeping your head elevated can help reduce this.
- Discomfort: Mild to moderate pain is common. Following your surgeon’s pain management plan, including prescribed medications, is crucial.
- Diet Changes: You may need to consume soft foods and liquids for a short duration. Avoiding strenuous chewing or hard foods helps in minimizing strain on the facial areas.
Returning to Normal Activities
The transition back to your normal lifestyle will be gradual. The length of this process can vary based on the complexity of the surgery. Generally, here’s what you can expect:
| Activity | Timeline |
|---|---|
| Light activities (reading, TV) | 1 week post-surgery |
| Return to work (sedentary) | 1-2 weeks post-surgery |
| Exercise (light cardio) | 4-6 weeks post-surgery |
| High-impact sports | 8-12 weeks post-surgery |
Patients should avoid strenuous activities or heavy lifting for at least four to six weeks, and it may also be advisable to avoid direct sunlight exposure to minimize discoloration during the early stages of recovery.
Follow-Up Appointments
Regular follow-up appointments with your surgeon are essential to monitor your healing progress and address any concerns that may arise. These visits will typically involve:
- Suture removal (if applicable) around 5-10 days post-operation
- Assessment of swelling and healing
- Adjustment of medication as needed
Emotional Adjustment
Lastly, it’s important to recognize that emotional adjustments are a part of the recovery. Feelings of anxiety or frustration are common, especially when you see changes in your appearance. Engaging with support groups or speaking with a mental health professional can be beneficial during this transition.
In summary, the recovery process after facial reconstruction surgery involves not just physical healing, but also emotional support and gradual reintegration into daily activities. Preparing for the ups and downs ahead is key to navigating this life-changing journey successfully.
Managing Pain and Discomfort After Surgery
Following facial reconstruction surgery, patients often experience varying degrees of pain and discomfort as part of their recovery journey. Efficient pain management is crucial for not only enhancing the patient’s comfort but also promoting healing and returning to everyday activities. Below, we explore various approaches to managing pain and discomfort in the post-surgical phase.
Understanding Pain After Surgery
Pain after facial reconstruction surgery can stem from several factors, including:
- Surgical Trauma: The procedure may involve cutting through skin, muscle, and tissue, which naturally generates pain as the body responds to the trauma.
- Swelling and Inflammation: Following surgery, inflammatory responses are triggered, leading to swelling that can exert pressure on surrounding structures.
- Nerve Activity: The manipulation and potential alteration of facial nerves can cause sensations of pain, tingling, or numbness.
Pain Management Strategies
A comprehensive pain management strategy encompasses various techniques as outlined in the table below:
| Pain Management Technique | Description |
|---|---|
| Medications | Post-operative medications may include prescribed opioids for immediate pain and over-the-counter anti-inflammatories for ongoing discomfort. |
| Cold Compresses | Applying a cold compress to the affected areas helps reduce swelling and numbs the area, providing immediate relief from discomfort. |
| Rest and Positioning | Adequate rest and proper head positioning during sleep help minimize strain on facial tissues, leading to decreased pain. |
| Breathing Techniques | Deep breathing exercises can promote relaxation and lower stress levels, which can positively influence pain perception. |
| Physical Therapy | Gentle exercises recommended by a therapist can gradually improve mobility and reduce stiffness without exacerbating pain. |
| Mindfulness and Relaxation Techniques | Practices such as meditation, guided imagery, or yoga may assist patients in managing pain by promoting mental well-being. |
Importance of Communication
Effective communication with healthcare providers about pain intensity and characteristics is critical. Patients should feel empowered to inform their medical team about any discomfort they are experiencing. Pain scales ranging from 1 to 10 can help describe pain levels more effectively, allowing for timely adjustments to pain management strategies.
Monitoring for Complications
While managing pain is essential, patients should also be vigilant for any signs of complications. Symptoms that may indicate issues include:
- Severe or Worsening Pain: If pain escalates or becomes irregular, it may signal an underlying complication, such as infection or abnormal healing.
- Discoloration or Unusual Swelling: Significant changes in skin color or excessive swelling can warrant immediate medical attention.
- Fever or Chills: These may indicate an infection, necessitating prompt evaluation by the healthcare team.
Conclusion
Knowing how to manage pain effectively after facial reconstruction surgery is an integral part of the healing process. By utilizing a combination of medications, physical support, communication, and mindfulness practices, patients can significantly enhance their recovery experience. Adequate pain management not only aids in physical healing but also plays a pivotal role in the overall psychological well-being, contributing to a smoother transition back to daily life.

Psychological Impact of Facial Trauma and Reconstruction
The realm of facial trauma encompasses not only the physical alterations that may occur due to accidents or medical conditions but also significant psychological ramifications. Individuals confronting facial trauma often experience a myriad of emotional responses that can affect their quality of life, self-esteem, and interpersonal relationships. Understanding these psychological impacts is crucial for both patients and healthcare providers involved in facial reconstruction surgery.
Emotional Response to Facial Trauma
Facial trauma can lead to a range of emotional reactions, including anxiety, depression, and post-traumatic stress disorder (PTSD). The visibility of facial injuries can make individuals feel vulnerable and exposed. Research indicates that the following emotional responses are common among patients:
| Emotional Impact | Description |
|---|---|
| Anxiety | Patients may fear social interactions or be concerned about judgment. |
| Depression | Loss of self-image can lead to feelings of hopelessness. |
| Post-Traumatic Stress | Flashbacks or intrusive thoughts related to the trauma experienced. |
Changes in Self-Perception
The face is a crucial aspect of personal identity. When injuries alter one’s appearance, it can drastically change how individuals perceive themselves. This altered self-image can lead to a withdrawal from social situations, causing isolation and exacerbating feelings of loneliness and despair. Psychologists emphasize the importance of addressing these changes proactively. Through therapeutic avenues, patients can work to reconstruct their self-image in tandem with physical restoration.
Importance of Psychological Support
After sustaining facial trauma, psychological support is essential. Counseling or therapy provides a safe space for individuals to express their feelings and develop coping strategies. Support from mental health professionals can help patients navigate the following challenges:
- Building Coping Mechanisms: Discovering healthy methods to deal with anxiety and emotional distress.
- Addressing Body Image Issues: Learning to accept new features and fostering a positive body image.
- Reintegration into Society: Developing strategies to re-engage socially and rebuild relationships.
Integrating Psychological Support in Recovery
For effective recovery, a holistic approach is vital. Here’s how psychological support can be integrated into facial reconstruction surgery treatment:
| Support Team Members | Role in Recovery |
|---|---|
| Psychologists/Therapists | Provide therapy to address emotional and psychological effects. |
| Surgeons | Communicate openly about expected outcomes and potential changes. |
| Support Groups | Offer shared experiences and a safe space for emotional expression. |
Collaborative engagement between these specialties can significantly enhance the recovery experience.
Success Through Support
Numerous testimonials from patients highlight the transformative power of addressing psychological aspects alongside physical recovery. Over time, individuals often find that engaging with mental health resources allows them to reclaim not just their appearance but also their confidence and social functionality. Patients who are well-prepped psychologically often report a smoother recovery process and higher satisfaction rates post-surgery.
Addressing the psychological impact of facial trauma and reconstruction should be a priority for anyone undergoing these procedures. Understanding the emotional journey involved fosters resilience, encouraging individuals to embrace their new selves with confidence and support.
Success Stories: Transformative Outcomes of Facial Reconstruction
Facial reconstruction surgery can lead to life-changing transformations for individuals who have endured trauma, congenital abnormalities, or severe injuries. The remarkable outcomes highlight not only the medical advancements in this field but also the profound emotional and psychological benefits for patients. Here, we explore various success stories that showcase the positive impact of facial reconstruction surgery.
Real-Life Transformations
- Rebuilding after Trauma
- Case Study: John
- Background: John, a 32-year-old cyclist, suffered a devastating accident that resulted in multiple facial fractures and significant tissue damage.
- Surgical Procedure: After thorough evaluation, John underwent a series of surgeries involving bone grafts and skin flaps. These techniques restored his facial structure and improved function.
- Outcome: Post-surgery, John regained full range of motion in his jaw and the ability to smile naturally, boosting his confidence and allowing him to return to his daily activities with renewed enthusiasm.
- Case Study: John
- Correcting Congenital Defects
- Case Study: Emily
- Background: Emily, born with a cleft lip and palate, faced social stigma and challenges with eating and speaking.
- Surgical Procedure: Multiple surgeries throughout her childhood included reconstructive procedures to close the cleft and align her jaw and teeth.
- Outcome: As an adult, Emily reported significant improvements in both her physical appearance and her self-esteem. Her ability to communicate clearly has opened new opportunities in her personal and professional life.
- Case Study: Emily
- Reconstruction after Cancer
- Case Study: Sarah
- Background: Sarah, a 45-year-old breast cancer survivor, faced the need for a mastectomy and subsequent facial surgery due to reconstruction-related complications.
- Surgical Procedure: Her treatment involved innovative microsurgery to reshape her facial contours and create a natural appearance, integrating skin from other areas of her body.
- Outcome: The transformative results allowed Sarah to embrace her new look, reinforcing her outlook on life and her battle against cancer. She became an advocate, sharing her journey to inspire others facing similar challenges.
- Case Study: Sarah
Comparative Outcomes
| Case Study | Issue Addressed | Type of Surgery | Key Outcome |
|---|---|---|---|
| John | Facial trauma | Bone graft and skin flap | Restored functionality and appearance |
| Emily | Cleft lip/palate | Reconstructive surgery | Enhanced self-esteem and communication |
| Sarah | Cancer reconstruction | Microsurgery | Empowered her advocacy and recovery |
The Essence of Transformation
The profound changes brought about by facial reconstruction surgery extend beyond physical results. Many patients report improvements in their quality of life, social interactions, and self-perception. These transformations serve as a testament to the delicate balance between art and science in surgical practices, demonstrating how skillful surgeons can restore harmony and address complex facial issues.
Ultimately, success stories like those of John, Emily, and Sarah illustrate the power of hope, resilience, and medical excellence. The advancements in surgical techniques and the commitment of dedicated teams have propelled countless individuals towards a brighter, more fulfilling future. As these stories circulate, they not only inspire others who have experienced similar challenges but also foster greater awareness and understanding of the vital role that facial reconstruction surgery plays in healing and restoration.
Future Innovations in Facial Reconstruction Surgery
The field of facial reconstruction is continually evolving, with groundbreaking innovations set to revolutionize the way specialists approach the restorative process. As technology advances and new methodologies emerge, medical professionals are poised to deliver even more effective solutions for individuals experiencing facial trauma or congenital abnormalities. Here are some of the most promising innovations on the horizon:
1. 3D Printing Technology
3D printing has begun to play a pivotal role in enhancing the precision and customization of surgical procedures. Surgeons can create patient-specific models based on CT or MRI scans, allowing for better preoperative planning. This technology enables professionals to practice complex operations on the printed models, ensuring more predictable outcomes.
Benefits of 3D Printing:
| Aspect | Advantages |
|---|---|
| Customization | Tailored implants and prosthetics |
| Surgical Simulation | Enhanced preoperative planning |
| Reduced Surgical Time | Streamlined procedures due to familiarity |
2. Regenerative Medicine
The integration of regenerative medicine within facial reconstruction offers an exciting frontier. Techniques such as stem cell therapy and tissue engineering can support the healing process and improve the integration of grafts. By harnessing the body’s natural healing abilities, these methods aim to restore both form and function more effectively.
Key Techniques:
| Technique | Description |
|---|---|
| Stem Cell Therapy | Utilizes the body’s own cells to repair tissue |
| Tissue Engineering | Combines cells and scaffolds to create new tissue |
3. Advanced Imaging Methods
Imaging technologies are evolving, making it easier for surgeons to visualize complex anatomical structures before initiating procedures. Innovations like augmented reality (AR) and virtual reality (VR) are being incorporated into surgical practices. Surgeons can visualize both the anatomy and the surgical plan in real time, which aids decision-making during operations.
4. Biodegradable Implants
The development of biodegradable materials for implants is altering the landscape of facial reconstruction. These implants offer the dual benefit of providing support during the healing phase while gradually dissolving, thus minimizing complications associated with long-term foreign bodies. Some of these materials can even promote tissue growth, enhancing healing outcomes.
Advantages of Biodegradable Implants:
| Feature | Benefits |
|---|---|
| Reduced Need for Removal | Eliminates a second surgery |
| Decreased Infection Risk | Lower chances of complications |
| Enhanced Healing Potential | Supports natural tissue regeneration |
5. Artificial Intelligence in Surgery
The incorporation of artificial intelligence (AI) in surgical planning and execution is another innovation transforming the field. AI algorithms can analyze vast amounts of data to identify risks, suggest surgical approaches, and even predict patient outcomes. Machine learning allows for continuous improvement of techniques and personalized care strategies.
6. Personalized Medicine
Personalized medicine focuses on tailoring treatments to individual genetic, environmental, and lifestyle factors. This burgeoning trend in facial reconstruction holds immense promise, as practitioners can develop targeted treatment plans that optimize results and align with the specific needs of each patient.
In summary, advancements in technology, materials science, and personalized care are coming together to shape the future of facial reconstruction. These innovations promise enhanced precision, improved outcomes, and a more compassionate approach to restoring both function and aesthetics for those impacted by trauma or congenital conditions. As this field continues to grow, the benefits of these technologies will likely extend beyond surgery, influencing recovery, rehabilitation, and overall quality of life for patients.

Frequently Asked Questions
What is facial reconstruction surgery?
Facial reconstruction surgery is a specialized surgical procedure aimed at restoring the appearance and functionality of the face after trauma, injury, or congenital defects. This type of surgery can address various issues, including fractures, soft tissue injuries, or disfigurements caused by accidents, tumors, or other medical conditions. The goal is to create a more harmonious and natural look, often involving the use of surgical techniques to reposition, graft, or rebuild facial structures.
Who is a candidate for facial reconstruction surgery?
Candidates for facial reconstruction surgery typically include individuals who have experienced significant facial injuries due to accidents, sports injuries, or violent incidents. Additionally, people born with congenital facial deformities or facial asymmetries may also seek this surgery. Candidates should be in good overall health and have realistic expectations about the outcomes of the procedure, as well as a willingness to undergo follow-up treatments or rehabilitation if necessary.
What can be expected during the recovery process?
Recovery from facial reconstruction surgery varies depending on the extent of the surgery performed but generally includes a period of swelling, bruising, and discomfort. Patients often need to follow specific postoperative care instructions, which may include rest, ice applications, and prescribed medications for pain management. Follow-up visits with the surgeon are essential to monitor healing progress and to address any complications. Most patients can return to regular activities within a few weeks, but full recovery may take several months.
How long does facial reconstruction surgery take?
The duration of facial reconstruction surgery can vary greatly based on the complexity of the case, the techniques used, and the specific areas of the face being addressed. On average, the procedure can take anywhere from a few hours to an entire day. More extensive reconstructions that involve multiple stages or extensive grafting may require additional time and possibly multiple surgeries spaced out over months. The surgeon will provide a more precise estimation during the consultation process.
Are there any risks associated with facial reconstruction surgery?
As with any surgical procedure, facial reconstruction surgery carries certain risks, including bleeding, infection, scarring, and anesthesia complications. Additionally, there may be risks specific to the surgical techniques used, such as nerve damage or dissatisfaction with cosmetic results. It is crucial for patients to have thorough discussions with their surgeon regarding these risks and to understand the safety measures in place to mitigate them, ensuring informed consent prior to proceeding with the surgery.