Gynecomastia, a condition characterized by enlarged male breast tissue, affects a significant number of men and can lead to considerable psychological distress. As societal standards shift and discussions around masculinity evolve, the importance of addressing this issue cannot be overstated. Many men find themselves struggling with self-esteem and confidence due to the physical appearance associated with gynecomastia. However, advancements in medical science offer various solutions that can help restore their confidence. In this blog post, we will explore the causes and symptoms of gynecomastia, the psychological effects it has on men, and a comprehensive overview of both surgical and non-surgical treatment options. By understanding the complete journey of gynecomastia removal, men can regain control over their bodies and enhance their overall quality of life.
Understanding Gynecomastia: Causes and Symptoms
Gynecomastia is a condition characterized by the enlargement of breast tissue in males, which can lead to physical discomfort and significant psychological distress. Understanding the causes and symptoms of gynecomastia is essential for recognizing the condition and seeking appropriate treatment. This section delves into the various factors contributing to gynecomastia and outlines the symptoms that individuals may experience.
Causes of Gynecomastia
Gynecomastia occurs due to an imbalance between estrogen and testosterone levels in the body. While males typically have higher testosterone levels, even minor fluctuations can catalyze the development of this condition. The following table highlights some common causes of gynecomastia:
| Cause | Description |
|---|---|
| Hormonal Changes | Puberty, men aging, and conditions affecting hormonal levels can lead to gynecomastia. |
| Medications | Certain medications such as anti-androgens, anabolic steroids, and some heart drugs. |
| Health Conditions | Conditions such as liver disease, hyperthyroidism, and tumors affecting hormone levels. |
| Substance Abuse | Use of substances like marijuana, alcohol, and opioids has been linked to gynecomastia. |
| Genetic Factors | Genetic predisposition and congenital disorders can contribute to abnormal breast tissue growth. |
Symptoms of Gynecomastia
Men affected by gynecomastia often experience both physical and emotional symptoms. The presence of excess breast tissue can lead to discomfort and self-consciousness. Below is a brief description of common symptoms associated with this condition:
- Swollen Breast Tissue: The most prominent symptom is an increase in the size of one or both breasts, which often feels firm and rubbery to the touch.
- Pain or Tenderness: Some individuals may experience soreness or tenderness in the breast area, which can cause discomfort during physical activities or when the area is touched.
- Sensitivity: Increased sensitivity around the chest area is often reported by those with gynecomastia, making it difficult to wear tight clothing or engage in certain sports.
- Psychological Effects: The emotional toll can be severe, leading to issues such as anxiety, depression, and social withdrawal. Many men may feel embarrassed, leading to a decline in self-esteem and confidence.
Recognizing Health Risks
Although gynecomastia is frequently a benign condition, it is crucial to consult a healthcare professional if symptoms persist. Recognizing potential underlying health issues is essential, as chronic gynecomastia may require medical intervention.
It is crucial to understand that gynecomastia can occur at various life stages, such as infancy, puberty, and later adulthood. Awareness of the causes and symptoms enables individuals to seek appropriate help early on, facilitating a more effective treatment process.
In summary, a comprehensive understanding of gynecomastia, its causes, and associated symptoms lays the foundation for men to acknowledge the condition and take proactive steps toward treatment. Being informed can pave the way for restoring not just physical appearance but also overall confidence in social settings.

The Psychological Impact of Gynecomastia on Men
Gynecomastia, the condition characterized by enlarged breast tissue in males, extends beyond physical implications, significantly influencing the psychological well-being of those affected. Understanding the psychological impact of this condition is essential, as it can lead to a substantial decrease in self-esteem, increased anxiety, and social withdrawal. Men suffering from this condition often require comprehensive support to navigate the emotional challenges that arise.
Emotional Responses
The emotional landscape of individuals coping with gynecomastia is complex. Common emotional reactions include:
- Embarrassment: Many men feel self-conscious about their appearance, particularly in situations where they are expected to remove their shirts, such as at the beach or during intimate moments.
- Low Self-Esteem: The visible effects of gynecomastia can lead to an unfavorable self-image, often translating into feelings of inadequacy or unworthiness.
- Depression and Anxiety: Persistent worries about body image can spiral into more severe mental health issues if not addressed. It is not uncommon for males with gynecomastia to experience episodes of depression, anxiety, or even social phobia.
Social Impact
The condition can hinder social relationships and personal interactions. Key points of social impact include:
| Area | Effects |
|---|---|
| Dating | Many men may avoid dating or intimacy due to insecurity about their bodies. |
| Friendships | Social gatherings can become daunting if a man feels exposed or judged by his peers. |
| Work Environment | The fear of being ridiculed can lead to an avoidance of professional situations, particularly those that involve client relations or public speaking. |
Coping Mechanisms
Men grappling with gynecomastia often develop various coping strategies, some of which may not be healthy. These can include:
- Clothing Choices: Many opt for loose-fitting or layered clothing to disguise the unwanted appearance of their breasts, which can inadvertently affect their overall style and comfort.
- Avoidance: Some individuals may withdraw from social situations or activities they once enjoyed, leading to isolation and further psychological distress.
- Increased Body Builder or Fitness Regimens: While exercise can be beneficial, some may take it to extremes to compensate for their body image issues, risking injury or burnout.
Seeking Help
Acknowledging the psychological impact of gynecomastia is essential in fostering recovery. Mental health professionals, such as therapists and counselors, can provide valuable support in the form of cognitive behavioral therapy (CBT) and other interventions aimed at addressing the emotional turmoil associated with the condition. Group therapy can also be helpful, as it allows individuals to connect with others who share similar experiences.
In addition to psychological support, consultations with healthcare professionals specializing in gynecomastia can create a personalized approach to treatment, combining both physical and emotional well-being. This multifaceted approach emphasizes that healing from gynecomastia is not solely about physical surgery but also involves a significant psychological component.
Ultimately, understanding the emotional ramifications of gynecomastia allows affected individuals to recognize that they are not alone in their struggles, paving the way for improved confidence and mental health. By addressing both the physical and psychological aspects, men can embark on a path towards genuinely restoring their self-esteem and quality of life.
Assessment and Diagnosis: What to Expect
When dealing with gynecomastia, understanding the assessment and diagnosis process is crucial for men experiencing this condition. It involves a comprehensive evaluation by a healthcare professional to determine the underlying causes and the most appropriate treatment options. This article will guide you through what you can expect during the assessment process.
Initial Consultation
The first step in assessing gynecomastia involves an initial consultation with a healthcare provider, often a specialist such as an endocrinologist or a plastic surgeon. During this meeting, you will discuss your medical history, including any medications you’re taking, past illnesses, family history of gynecomastia, and lifestyle factors that might contribute to the condition.
Key discussion points may include:
| Category | Details |
|---|---|
| Medical History | Review of past and current health issues |
| Medication Review | Analysis of medications and supplements |
| Lifestyle Factors | Assessment of diet, exercise, and alcohol use |
| Family History | Possible genetic predisposition |
This thorough dialogue aids in pinpointing whether gynecomastia is a result of hormonal imbalances, medications, or other medical conditions.
Physical Examination
Following the consultation, a physical examination will be conducted. In this step, the healthcare professional will visually inspect and palpate the breast tissue to evaluate the size and characteristics of the breasts. They may also assess for any discomfort or tenderness present in the chest area.
Physical Examination Focus Areas:
- Breast Tissue Characteristics: Determining if breast tissue is firm, soft, or swollen.
- Symmetry: Checking the uniformity of both breasts to identify any significant disparities.
- Signs of Other Conditions: Looking for possible indicators of larger medical issues or hormonal imbalances.
Diagnostic Tests
In some cases, further diagnostic tests may be necessary to confirm the diagnosis or rule out other medical conditions. These tests can include:
- Blood Tests: To evaluate hormone levels, particularly testosterone and estradiol. Changes in these levels can indicate hormonal imbalances.
- Imaging Studies: Such as mammograms or ultrasounds. These imaging tests are utilized to assess breast tissue and determine whether the mass is glandular (gynecomastia) or fatty (lipomastia).
- Tissue Biopsy: Rarely, a biopsy may be performed to rule out any malignant conditions.
Understanding the Diagnosis
Once all assessments and tests have been completed, your healthcare provider will explain the findings and provide an accurate diagnosis. Gynecomastia may be classified into several types based on its causes:
| Type | Description |
|---|---|
| Pubertal Gynecomastia | Common during puberty; usually resolves on its own. |
| Physiological Gynecomastia | Commonly occurs due to hormonal changes associated with aging. |
| Pathological Gynecomastia | Resulting from medical conditions or medications. |
Understanding the type of gynecomastia can help determine the recommended course of action. If the condition is due to hormonal imbalances or removable factors, non-surgical options and lifestyle changes may be suggested. Conversely, if surgical intervention is warranted, the healthcare provider will discuss possible operating techniques and expected outcomes.
Moving Forward
The assessment and diagnosis process for gynecomastia is a pivotal step in the journey toward rebuilding confidence. Engaging in a complete understanding of the medical conditions, treatment options, and potential outcomes helps empower men to take effective steps in addressing this challenging condition. Remember, early intervention can lead to more favorable results, allowing for timely diagnosis and treatment tailored to individual needs.
Preparing for Gynecomastia Surgery
Undergoing surgery is a significant step in anyone’s life, particularly for those seeking gynecomastia removal. Proper preparation ensures the procedure proceeds smoothly and contributes to a successful recovery. Hence, it is crucial to understand the various aspects involved in preparing for the surgery.
Initial Consultation with a Surgeon
Before the actual surgical procedure, a consultation with your surgeon is imperative. During this appointment, you will discuss your medical history, any medications you currently take, and the specific goals for the surgery. It’s an excellent opportunity to clarify any questions or concerns you may have. Additionally, your surgeon will conduct a physical examination to evaluate the extent of gynecomastia and gauge the best surgical method for your needs.
Medical Clearance and Preoperative Testing
Most surgeons will require a medical clearance before proceeding. This can include blood tests, an ECG (Electrocardiogram), or other diagnostic tests to assess your overall health. If you have any existing health conditions such as heart disease, diabetes, or hypertension, it is crucial to ensure they are well-managed before surgery. The preoperative testing may vary depending on your age and individual health status.
| Test Type | Purpose | Common Requirements |
|---|---|---|
| Blood Tests | Assess general health and identify risks | Fasting may be required |
| ECG | Evaluate heart function | Typically non-invasive |
| Physical Exam | Review health history | Comprehensive assessment |
Lifestyle Modifications
Leading up to the surgery, certain lifestyle modifications can aid in a smoother surgical experience. These changes often involve:
- Dietary Adjustments: Maintaining a balanced diet that includes plenty of fruits, vegetables, and lean proteins can boost your overall health and assist in recovery. Limiting alcohol and processed foods, especially in the week leading to surgery, is advisable.
- Smoking Cessation: Smoking can significantly affect circulation and healing capabilities. If you are a smoker, your surgeon may recommend quitting at least four to six weeks before the procedure.
- Exercise Regimen: While maintaining a regular exercise routine is generally beneficial, it’s essential to scale it back as the surgery date approaches. Engaging in high-intensity workouts immediately prior to surgery can lead to fatigue and stress on the body.
Medications and Supplements
Before surgery, it is crucial to inform your surgeon about all medications and dietary supplements you are taking. Certain medications, especially blood thinners like aspirin or ibuprofen, need to be avoided as they can increase bleeding risk during surgery. Your surgeon may recommend a specific discontinuation schedule.
Arranging Support for Surgery Day
On the day of the surgery, having a support system in place is vital. Plan to have someone with you to help with transportation to and from the surgery center. Post-operative recovery may include grogginess from anesthesia, so arranging care for the first 24-48 hours is essential.
| Preparation Checklist | Description |
|---|---|
| Transportation Arranged | Ensure someone can drive you home |
| Post-Op Care | Have someone to help with basic needs |
| Extended Recovery Support | Prepare for assistance in the following days |
In summary, thoroughly preparing for gynecomastia surgery involves multiple steps, including consultations, medical testing, lifestyle changes, medication management, and arranging support. Each of these elements plays an important role in ensuring a smoother process and fostering positive surgical outcomes. By taking these steps seriously, individuals can enhance their overall experience and pave the way for renewed confidence following surgery.

The Recovery Process: What to Anticipate
Undergoing surgery can be both exciting and daunting. For men pursuing gynecomastia removal, understanding the recovery process is crucial to ensuring a smooth transition back to daily activities. Recovery timelines can vary based on the individual, the type of surgical procedure performed, and overall health. Here’s what to expect during the recovery period:
Immediate Post-Operative Care
After the procedure, patients typically spend some time in a recovery room under observation before being discharged. It’s common to experience:
- Swelling and Discomfort: The chest area may feel swollen and tender. Your surgeon may prescribe pain medication to manage discomfort.
- Compression Garments: Patients are usually instructed to wear a compression garment for a specified duration to minimize swelling and support the healing tissues.
First Week Post-Surgery
During the initial week, patients should plan to focus on rest and recovery. Doctors usually provide specific instructions regarding activity levels. Key points to consider include:
| Activity | Recommendation |
|---|---|
| Physical Activity | Avoid any strenuous exercises or lifting heavy objects for at least two weeks. |
| Work Commitments | Many patients can return to light desk jobs within a few days; however, more strenuous jobs may require longer recovery. |
| Showering | Usually, showering is permitted after 24-48 hours, but avoid soaking the surgical site. |
| Driving | Avoid driving until cleared by a healthcare provider, especially if pain medications are taken. |
| Diet | Maintain a healthy diet to support healing, focusing on protein-rich foods like lean meats, nuts, and dairy. |
Emotional Well-Being
Psychological recovery is just as important as physical healing. It’s common to experience a mix of emotions, including anxiety, excitement about the physical changes, and fears regarding the final results. Consider connecting with support groups or speaking with a mental health professional if needed.
Week Two to Four
As you enter the second week, symptoms such as swelling and bruising generally begin to subside. Here are some common experiences during this phase:
- Increased Mobility: Patients can usually resume normal activities, but should still be cautious with intense workouts and physical sports.
- Follow-Up Appointment: A follow-up visit with the surgeon is essential for checking healing progress and addressing any concerns.
Long-term Recovery
The complete healing process can take several months. By six weeks post-surgery, most patients can return to their typical exercise routines. However, final results may not be fully visible until three to six months after surgery.
Monitoring Changes
It is essential to regularly monitor the surgical site for any unusual changes, such as:
| Warning Signs | Description |
|---|---|
| Excessive Swelling | Persistent swelling beyond normal recovery times. |
| Discharges | Any unusual drainage or strong odors from the incision site could indicate infection. |
| Severe Pain | Intense pain that isn’t alleviated by prescribed medication should be assessed. |
Importance of Following Medical Advice
Adhering closely to the post-operative guidelines provided by your surgeon will be vital for preventing complications and ensuring optimal results. Make sure to attend all scheduled follow-up appointments and communicate openly about any concerns you may have regarding your recovery.
By proactively managing your recovery process, you can effectively reduce discomfort and facilitate a smooth transition back to your regular lifestyle, paving the way towards restored confidence and improved self-image.
Risks and Complications of Gynecomastia Surgery
Undergoing surgery for gynecomastia is a significant step in reclaiming confidence and enhancing personal aesthetics for many men. However, like any surgical procedure, it comes with its own set of risks and potential complications that individuals should be fully aware of before making a decision. Understanding these factors can help set realistic expectations and prepare for a smoother recovery.
Common Risks Associated with the Surgery
Below is a detailed table that outlines the most prevalent risks and complications associated with gynecomastia surgery:
| Risk | Description |
|---|---|
| Infection | Surgery can introduce bacteria into the body, leading to infections. Symptoms may include redness, swelling, and fever. Antibiotics are often prescribed to mitigate this risk. |
| Scarring | Surgical incisions may lead to noticeable scars, particularly in cases of extensive tissue removal. Proper post-operative care can help minimize this complication. |
| Bleeding (Hematoma) | Excessive bleeding during or after the procedure can result in a hematoma, requiring additional intervention to correct. |
| Asymmetry | Results may vary, leading to uneven contours in the chest area. This can necessitate revision surgery if the disparity is significant. |
| Nipple Sensitivity Changes | Some patients experience altered sensation in the nipple area, ranging from heightened sensitivity to numbness. These changes can be temporary or, in rare cases, permanent. |
| Fluid Accumulation (Seroma) | The accumulation of fluid beneath the skin can occur, requiring drainage. Proper surgical technique and aftercare are crucial to prevent seromas. |
| Delayed Healing | Some individuals may experience delayed healing, especially if they have underlying health conditions or are smokers, which could impact recovery. |
| Anesthesia Risks | General anesthesia carries its own risks, including respiratory issues or allergic reactions. An experienced anesthesiologist can help mitigate these concerns. |
Understanding the Psychological Impact
In addition to the physical risks, it’s crucial to consider the psychological ramifications that may arise after surgery. Patients might face anxiety, depression, or issues with body image if the results do not meet their expectations. It is essential for individuals to have realistic goals and to discuss any concerns with their surgeon during pre-operative consultations.
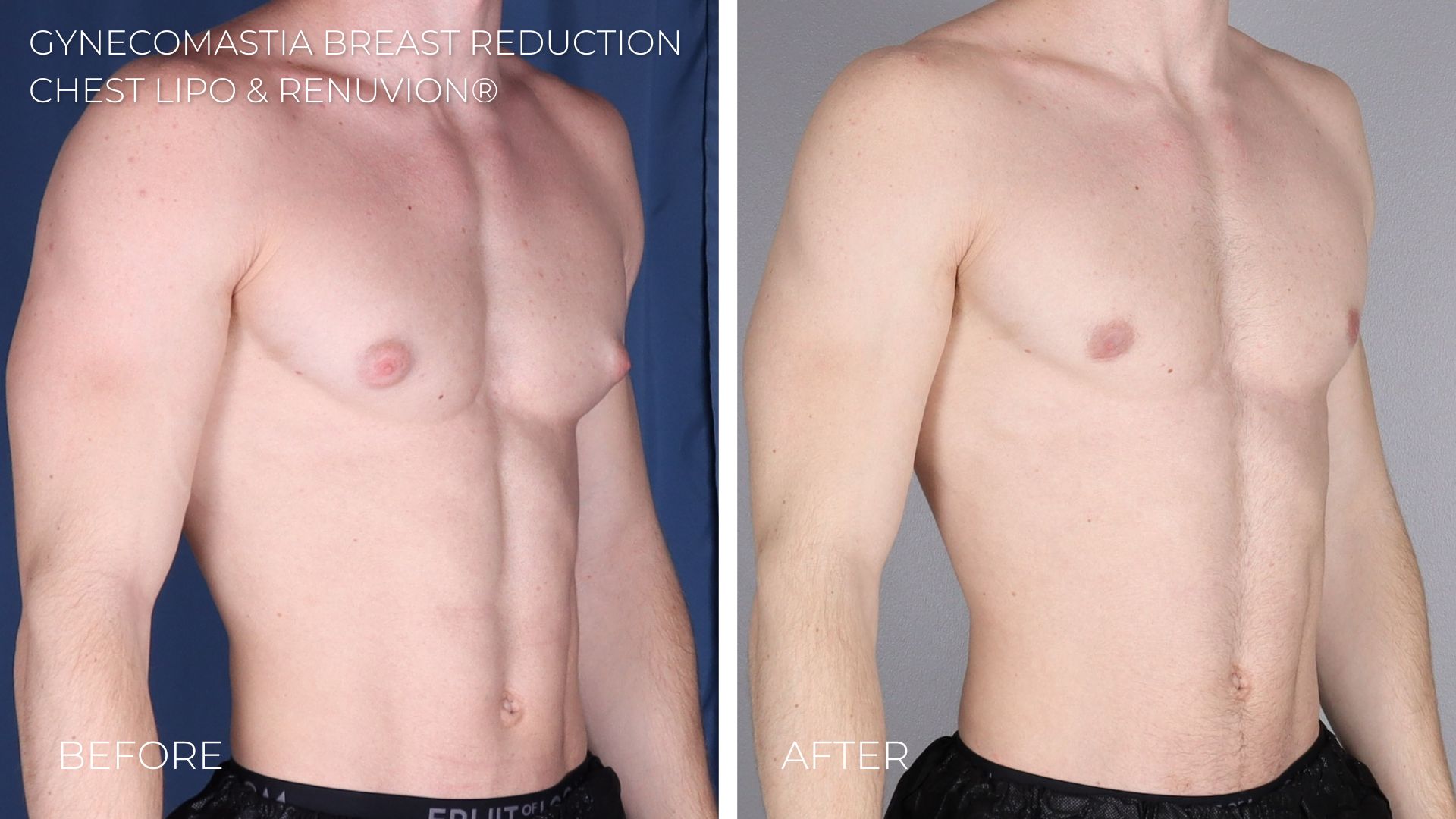
Importance of Selecting a Qualified Surgeon
Choosing a board-certified plastic surgeon with extensive experience in gynecomastia procedures is vital. A qualified professional can minimize surgery risks by employing proper techniques, ensuring safe practices, and providing comprehensive pre- and post-operative care. Consulting with past patients and examining before-and-after photos can instill confidence in one’s choice of a surgeon.
Post-Operative Care and Vigilance
After the surgical procedure, adhering to post-operative care instructions is crucial for mitigating risks. This may include:
- Wearing compression garments to reduce swelling and support healing.
- Avoiding vigorous activities for several weeks to prevent complications such as bleeding or fluid accumulation.
- Monitoring for unusual symptoms, such as increased pain or redness, which may indicate complications.
Prompt communication with your healthcare provider about any concerns can help catch issues early and enhance recovery.
In summary, while the journey to removing gynecomastia can be transformative, it is essential to approach it with careful consideration of the potential risks and complications involved, along with proactive measures to ensure a successful outcome. Engaging with a knowledgeable surgical team and maintaining a commitment to personal health and safety can significantly bolster the chances of achieving a positive experience and result.
Cost Considerations for Gynecomastia Removal
Understanding the financial implications of surgical interventions for gynecomastia is essential for anyone considering this transformative procedure. The costs associated with gynecomastia removal can vary widely based on multiple factors, including the type of surgery, geographical location, experience of the surgeon, and the complexity of the case. Below, we explore these elements in detail to provide you with comprehensive insights into the financial aspects of gynecomastia treatment.
Factors Influencing the Cost of Gynecomastia Removal
- Type of Surgery: There are different surgical techniques available for gynecomastia removal, and each has its own price point. The common procedures include:
| Surgical Procedure | Estimated Cost |
|---|---|
| Liposuction | $2,000 – $5,000 |
| Glandular excision | $3,500 – $7,000 |
| Combination of liposuction and excision | $4,000 – $8,000 |
- Geographical Location: The cost of living in various regions directly affects healthcare prices. Urban areas generally charge more due to higher overhead costs. As a reference, states like California and New York tend to have higher fees compared to less populated areas.
- Surgeon’s Expertise: Board-certified plastic surgeons with significant experience in gynecomastia procedures may command higher fees due to their skill level and the quality of results delivered. While it may be tempting to opt for a less expensive surgeon, the quality of care and potential for complications should guide this decision.
- Facility Fees: The surgical facility’s reputation and amenities can also impact costs. Hospitals with advanced technology and post-operative care options might charge more but can offer a higher level of care and comfort.
- Anesthesia: The type of anesthesia used during the procedure, whether local or general, will also influence the overall cost. General anesthesia may carry additional fees compared to local anesthesia due to the involvement of an anesthesiologist.
Additional Costs to Consider
It’s essential to be aware that the total cost of gynecomastia removal does not necessarily end with the surgeon’s fee. Additional costs may include:
- Pre-operative consultations: Initial assessments may incur fees that, while usually minor, can add up.
- Post-operative care: Follow-up visits, medication for pain management, and compression garments required after the surgery should be factored in.
- Scarring treatments: If you desire to reduce the appearance of scars post-surgery, treatments may also incur additional expenses.
Insurance Coverage for Gynecomastia Removal
Health insurance providers often view gynecomastia removal as a cosmetic procedure, leading to limited coverage options. However, if the condition causes significant psychological distress or physical discomfort, acquiring partial coverage is sometimes feasible. Consulting with a qualified insurance advisor can provide clarity on potential reimbursement for the procedure.
Financial Planning for Your Surgery
Considering the financial aspect of gynecomastia removal is vital for effective planning. It’s advisable to:
- Budget: Create a detailed budget that includes all anticipated costs.
- Explore financing options: Many facilities offer payment plans, allowing you to spread costs over time. This financial flexibility can make the procedure more accessible.
- Seek multiple quotes: Consult with several surgeons to compare costs and services offered. This process also enables you to gauge the surgeon’s suitability and overall approach to your case.
Understanding these cost considerations can empower individuals suffering from gynecomastia to make informed decisions, paving the way towards enhanced self-esteem and confidence.
Frequently Asked Questions
What is gynecomastia and what causes it?
Gynecomastia is a medical condition characterized by the enlargement of breast tissue in males. It can result from hormonal imbalances, particularly between testosterone and estrogen. Various factors can lead to these imbalances, including puberty, aging, certain medications, hormonal disorders, and lifestyle factors such as obesity or substance abuse. Understanding the underlying cause is crucial for determining the suitable treatment.
What are the treatment options for gynecomastia?
Treatment options for gynecomastia may vary based on the severity of the condition and its underlying causes. Non-surgical options include observation and lifestyle changes, like exercise and weight loss. Surgical options involve procedures such as liposuction or mastectomy to remove excess breast tissue. Hormonal treatments may also be considered in some cases, depending on the diagnosis. Consulting a healthcare professional will help determine the most appropriate treatment plan.
What can I expect during the gynecomastia surgery recovery process?
Recovery from gynecomastia surgery typically involves a period of rest and adherence to post-operative care guidelines. Patients may experience swelling, bruising, and discomfort, which can be managed with prescribed pain medications. Most individuals can resume normal activities within a week, though strenuous activities should be avoided for several weeks. Follow-up appointments are essential for monitoring the healing process and ensuring optimal results.
Will gynecomastia surgery leave scars?
Gynecomastia surgery will result in some degree of scarring, as it involves making incisions to remove excess tissue. However, a skilled surgeon will place incisions in discreet areas, such as along the natural contours of the breast or in areas where they are less visible. Over time, these scars typically fade and become less noticeable, but the extent of scarring will depend on the surgical technique used and the individual’s healing process.
How does gynecomastia surgery impact a man’s confidence and body image?
Undergoing gynecomastia surgery can have a profound impact on a man’s confidence and body image. Many men report significant improvements in their self-esteem, social interactions, and overall quality of life after the procedure. By addressing physical insecurities, individuals often feel more comfortable in social settings, engage in activities they previously avoided, and experience a renewed sense of masculinity and confidence in their appearance.