In the intricate world of healthcare, few specialists play as pivotal a role as the HPB surgeon when it comes to hepatopancreatobiliary procedures. These dedicated professionals are trained to handle complex surgical conditions affecting the liver, pancreas, and bile ducts, making them essential in treating a range of diseases. In this blog post, we will explore the critical functions of HPB surgeons in patient care, delve into the common conditions they address, and highlight the innovative surgical techniques that are transforming treatment outcomes. Moreover, we will discuss the importance of teamwork in healthcare, recovery and follow-up processes, and the provocative challenges faced within this specialty. With patient testimonials and success stories woven throughout, this comprehensive guide aims to equip you with the knowledge needed to choose the right HPB surgeon for your specific needs.
Role of HPB Surgeons in Patient Care
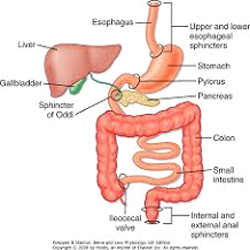
HPB surgeons, short for hepatopancreatobiliary surgeons, are specialized medical professionals who play a crucial role in the diagnosis, treatment, and management of diseases affecting the liver, pancreas, and biliary system. Their dedicated expertise not only enhances surgical outcomes but also significantly improves the overall patient experience. Below, we dive deep into the multifaceted role of these surgeons in patient care, outlining their responsibilities and the impact they have on the treatment journey.
Key Responsibilities of HPB Surgeons
The role of HPB surgeons involves a comprehensive range of responsibilities that extend beyond the operating room. This includes assessing patients for surgery, conducting complex surgical procedures, and providing ongoing care post-operation. Here’s a breakdown of their essential duties:
| Responsibility | Description |
|---|---|
| Preoperative Assessment | HPB surgeons evaluate patients through thorough medical history reviews, imaging studies, and laboratory tests, ensuring each individual is a suitable candidate for surgery. |
| Surgical Intervention | They perform intricate surgical procedures, including resections, transplants, and minimally invasive techniques, tailored to the specific condition and needs of the patient. |
| Multidisciplinary Teamwork | HPB surgeons frequently collaborate with oncologists, gastroenterologists, radiologists, and other specialists to devise a comprehensive treatment plan for each patient. |
| Patient Education | They educate patients about their conditions, treatment options, and possible outcomes, helping patients to make informed decisions regarding their care. |
| Postoperative Management | After surgery, HPB surgeons monitor recovery, manage pain, and address potential complications, ensuring a smooth recovery process and optimal outcomes. |
| Long-term Follow-up | They conduct regular follow-up visits to assess long-term health, manage any recurrent issues, and adjust treatment plans as necessary. |
Impact on Patient Outcomes
HPB surgeons directly influence the success rates of hepatopancreatobiliary procedures. By leveraging their specialized knowledge and skills, they help to minimize surgical risks and enhance recovery times. Additionally, effective communication and care coordination led by these surgeons can significantly increase patients’ confidence and satisfaction throughout their treatment journey.
Holistic Approach to Care
One of the main advantages of HPB surgeons is their focus on a holistic approach to patient care. This includes:
- Psychosocial Support: Recognizing that surgery can be a stressful experience, HPB surgeons often facilitate access to mental health resources and support groups.
- Nutritional Guidance: These specialists may also collaborate with dietitians to create nutritional plans that promote healing and overall well-being post-surgery.
- Lifestyle Modifications: HPB surgeons often advise patients on lifestyle changes tailored to their specific needs, such as exercise regimens and dietary adjustments designed to lessen the risk of future complications.
Building Trust through Communication
Effective communication is paramount in the relationship between HPB surgeons and their patients. By maintaining open lines of communication, they ensure that patients feel comfortable discussing their concerns and that any questions are adequately addressed. This trust contributes significantly to improved patient satisfaction and adherence to treatment plans.
In summary, HPB surgeons fulfill a multifaceted and vital role in patient care, allowing them to enhance treatment outcomes, improve patient experiences, and foster a supportive healthcare environment. Their expertise is essential in navigating the often complex journey of patients with hepatopancreatobiliary conditions.

Common Conditions Treated by HPB Surgeons
Hepatopancreatobiliary (HPB) surgeons are specialized medical professionals dedicated to diagnosing and treating a range of complex conditions related to the liver, pancreas, and bile ducts. These conditions often require expert intervention due to their intricate nature and the critical functions these organs perform in the human body. Understanding the common conditions treated by HPB surgeons can empower patients to seek timely and effective care. Below is a detailed overview of some prevalent disorders that fall under the purview of HPB surgery.
Liver Diseases
The liver is a vital organ responsible for various metabolic processes, and its diseases can significantly impact overall health. Some common liver conditions treated include:
| Condition | Description |
|---|---|
| Hepatocellular Carcinoma | A primary liver cancer that arises from liver cells, often associated with cirrhosis. |
| Liver Cirrhosis | Scarring of the liver tissue resulting from chronic liver disease, affecting liver function. |
| Liver Cysts | Fluid-filled sacs that can form in the liver, often asymptomatic but can require surgical intervention if large. |
| Liver Abscess | A collection of pus within the liver, typically caused by infection and requiring drainage. |
Pancreatic Disorders
The pancreas plays a crucial role in digestion and blood sugar regulation. HPB surgeons often address conditions such as:
| Condition | Description |
|---|---|
| Pancreatic Cancer | A malignant tumor that affects the pancreas, often diagnosed at an advanced stage. |
| Acute Pancreatitis | Sudden inflammation of the pancreas, commonly due to gallstones or alcohol intake. |
| Chronic Pancreatitis | Long-standing inflammation that results in pancreatic damage and insufficiency. |
| Pancreatic Cysts | Fluid-filled sacs on or within the pancreas that may need to be surgically removed. |
Bile Duct Obstructions
Bile ducts are essential for the transport of bile, and obstructions can lead to severe complications. Conditions managed by HPB surgeons in this area include:
| Condition | Description |
|---|---|
| Cholangiocarcinoma | A rare bile duct cancer that can lead to bile duct obstruction and liver problems. |
| Biliary Strictures | Narrowing of the bile duct, often due to injury, cancer, or inflammation, requiring surgery to alleviate the blockage. |
| Gallbladder Disease | Conditions like gallstones or inflammation that can affect bile flow. Surgical intervention may be necessary. |
Other Relevant Conditions
Beyond the primary organ-focused diseases, HPB surgeons also treat conditions that can complicate or involve multiple simultaneously affected organs:
| Condition | Description |
|---|---|
| Hemochromatosis | A genetic condition leading to excess iron accumulation in the liver, which can harm the organ. |
| Fatty Liver Disease | Excess fat accumulation can lead to inflammation and liver damage, necessitating surgical options in severe cases. |
| Portal Hypertension | Increased pressure in the portal vein often caused by liver cirrhosis, which may require surgical solutions like shunt placement. |
Final Thoughts
HPB surgeons are uniquely equipped to handle a diverse array of conditions affecting critical digestive organs. By employing advanced surgical techniques, these specialists can provide targeted treatments aimed at improving patient outcomes. When faced with symptoms or diagnoses related to the liver, pancreas, or bile ducts, early intervention by an HPB surgeon can be pivotal in managing these conditions successfully. Overall, understanding the various conditions treated provides a clearer picture of the role these skilled professionals play in healthcare.
HPB Surgical Techniques and Innovations
Hepatopancreatobiliary (HPB) surgery requires precision, expertise, and a sophisticated understanding of anatomy and pathology. Surgeons in this specialized field utilize a variety of surgical techniques, many of which have seen significant innovations in recent years, enhancing their effectiveness and patient outcomes. Here’s a comprehensive look at the current technologies and techniques employed in HPB surgery.
Key Surgical Techniques
- Open Surgery vs. Minimally Invasive Surgery
Traditionally, HPB surgeries were performed through open procedures requiring large incisions. However, advancements in surgical techniques have led to the proliferation of minimally invasive approaches, such as laparoscopic and robotic-assisted surgeries. These methods offer reduced recovery times and minimized post-operative pain.Procedure Type Description Advantages Open Surgery Involves significant incision and direct access to organs Comprehensive access; suitable for complex cases Laparoscopic Surgery Uses small incisions with a camera and instruments Less pain; shorter recovery time Robotic-Assisted Surgery Enhanced precision through robotic arms Greater dexterity; improved visualization - Liver Resection Techniques
Resection is a common procedure in HPB surgery, particularly for liver tumors. Surgeons employ various methods such as anatomic resection, where specific sections of the liver are removed, and non-anatomic resection, where the tumor is excised indiscriminately. Innovations like preoperative imaging and intraoperative ultrasound facilitate precise tumor localization before surgery. - Pancreaticoduodenectomy (Whipple Procedure)
The Whipple procedure is a complex operation primarily performed for pancreatic cancer. This technique has undergone significant refinement, with recent innovations enabling surgeons to perform this operation with lower complication rates. Surgeons now incorporate advanced imaging and reconstructive techniques that allow them to spare certain critical structures while removing cancerous tissues. - Biliary Reconstruction Techniques
After bile duct resection or injury, biliary reconstruction is crucial for restoring bile flow. Recent approaches, such as the use of biliary stents or anastomoses using advanced suture materials, have improved patient outcomes significantly. The development of tissue engineering techniques aims to enhance the effectiveness of these reconstructions, reducing complications associated with bile leaks.
Technological Innovations
The landscape of HPB surgery is dramatically shifting due to technology. Here are some highlights:
- Enhanced Visualization Tools: Techniques such as fluorescence imaging have emerged, where fluorescent dyes are used to visualize tumors, bile ducts, and vascular structures, assisting surgeons during procedures.
- 3D Printing: Customized 3D-printed organ models help surgeons plan complex procedures more effectively by simulating the operative field before making any incisions.
- Surgical Navigation Systems: Advanced software provides real-time guidance during surgery, ensuring that surgeons make the most informed decisions possible.
Patient-Specific Innovations
In addition to refined surgical techniques, personalized medicine has made inroads into HPB surgery. Genetic profiling and biomarker analysis allow for tailored postoperative management plans that can reduce the risk of recurrence in cancer patients, provide better pain management strategies, and inform the decision-making process for further treatments.
These advancements in HPB surgical techniques and innovations represent a commitment to continuous improvement and optimal patient care. As technologies evolve and new strategies are developed, HPB surgeons remain at the forefront of surgical excellence, improving the lives of patients with complex hepatopancreatobiliary conditions.
The Importance of Multidisciplinary Collaboration
In the realm of hepatopancreatobiliary (HPB) surgery, the significance of multidisciplinary collaboration cannot be overstated. This approach integrates expertise from various medical specialties, ensuring comprehensive and effective patient care throughout the entire treatment process. A collaborative framework not only enhances the quality of care but also contributes to improved patient outcomes and a more efficient healthcare delivery system.
Key Benefits of Multidisciplinary Collaboration
The following table summarizes the core benefits of adopting a multidisciplinary approach in HPB surgery:
| Benefit | Description |
|---|---|
| Holistic Patient Care | Integration of diverse medical perspectives helps address all aspects of a patient’s condition. |
| Enhanced Decision-Making | Input from various specialists leads to more informed clinical decisions tailored to individual needs. |
| Improved Communication | Ongoing discussions amongst specialists promote clearer communication of treatment plans to patients. |
| Comprehensive Management | Combines surgical expertise with nutritional, psychological, and rehabilitative support post-surgery. |
| Increased Research and Innovation | Collaborative efforts can spur innovative treatment protocols and encourage participation in clinical trials. |
The holistic care model is at the heart of multidisciplinary collaboration. Patients facing surgery for liver, pancreas, or biliary tract conditions often have complex medical histories. Bringing together specialists—such as hepatologists, oncologists, radiologists, nutritionists, and anesthesiologists—fosters a comprehensive evaluation of the patient’s health. This team-oriented approach allows for individualized treatment plans that accommodate various needs beyond surgical intervention.
Enhanced Decision-Making
In HPB surgery, correct diagnosis and timely intervention are crucial. Collaboration encourages collective insight from various medical professionals. For example:
- Hepatologists offer expert knowledge of liver diseases, critical for understanding pre-existing conditions that could complicate surgery.
- Radiologists provide advanced imaging techniques, which can be essential to ascertain the exact location and size of tumors or lesions.
- Anesthesiologists play a vital role in assessing patients’ readiness for anesthesia, especially in surgeries with elevated risks due to liver dysfunction.
This multidisciplinary exchange ultimately leads to high-quality and informed clinical decision-making. It helps in determining the most appropriate surgical techniques or alternative therapies.
Improved Communication
Patients often have questions or concerns regarding their diagnosis and treatment pathway. Multidisciplinary teams facilitate communication by ensuring that all specialists are on the same page, allowing for succinct and consistent messaging to the patient. Regular meetings and updates among clinicians ensure that care plans are well-coordinated, enhancing patients’ understanding and trust in the treatment they are receiving.
Comprehensive Management
The journey doesn’t end with surgical intervention. Post-operative care provided through multidisciplinary collaboration focuses on:
- Nutrition: Nutritionists assess dietary requirements, as patients need to be fortified alongside their recovery.
- Psychological Support: Mental health professionals can help patients cope with the emotional aspects of illness and surgery.
- Rehabilitation Services: Physical therapists guide patients in regaining strength and mobility post-surgery.
This comprehensive, wraparound approach not only optimizes recovery times but also improves overall quality of life after surgery.
In summary, the role of multidisciplinary collaboration in the field of HPB surgery forms the backbone of patient-centered care. By weaving together expertise from various specialties, it enhances the treatment protocol, ensuring that all aspects of a patient’s health are considered for an optimal recovery trajectory. The undeniable advantages of this collaborative approach pave the way for better surgical outcomes and higher patient satisfaction, making it a cornerstone in modern hepatopancreatobiliary procedures.
Recovery and Follow-Up Care after HPB Surgery
Recovering from hepatopancreatobiliary surgery is a vital part of the treatment journey, extending beyond the operating room and significantly impacting a patient’s overall health and quality of life. This phase involves meticulous attention to detail, requiring both medical expertise and patient commitment to ensure optimal outcomes.
Immediate Postoperative Care
After the surgery, patients are usually transferred to a recovery unit where they are closely monitored. Here, healthcare professionals check vital signs such as heart rate, blood pressure, and oxygen levels. Controlling pain levels, especially after a potentially invasive procedure, is crucial. Methods include:
- Pain Management Regimens: Administering medications through intravenous (IV) routes, moving to oral medications as soon as possible.
- Fluid Management: Patients may receive fluids through an IV to maintain hydration and electrolyte balance.
- Diet Progression: Initially, only clear liquids are permitted, gradually leading to a soft diet based on individual tolerance.
In-Hospital Stay Duration
The average hospital stay for HPB procedures can vary depending on the type of surgery performed. The following table highlights typical durations based on common procedures:
| Procedure Type | Average Hospital Stay |
|---|---|
| Laparoscopic Cholecystectomy | 1-2 days |
| Whipple Procedure | 5-7 days |
| Liver Resection | 5-10 days |
Patients can advance to a home setting once they display stable vital signs, manage to consume liquids without complications, and show adequate pain control.
Transitioning to Home Care
Post-discharge, the responsibilities increase for both healthcare providers and the patients themselves. Here are critical considerations for effective recovery at home:
- Wound Care: Keeping the surgical site clean and dry is essential. Patients should be educated on how to recognize signs of infection, such as increased redness, swelling, or drainage.
- Activity Level: Light physical activity is encouraged to promote circulation, although patients should avoid strenuous activities and heavy lifting for a specified period, usually three to six weeks post-surgery, depending on the procedure.
- Monitoring Symptoms: Patients must be vigilant about any changes in their condition. Common issues to watch for include fever, persistent abdominal pain, nausea, vomiting, and changes in bowel movements.
Follow-Up Appointments
Routine follow-up visits with the conducting HPB specialist are essential after discharge to:
- Assess Recovery Progress: These visits typically occur within 1-2 weeks post-surgery, allowing the surgeon to evaluate healing and adjust medications if necessary.
- Imaging Tests: Sometimes, imaging scans (like ultrasounds or CT scans) are conducted to monitor surgical outcomes, particularly in liver and pancreatic operations.
- Nutritional Guidance: As dietary changes are often required post-surgery, consultations with a nutritional specialist can help manage digestive modifications and incorporate a balanced diet.
Long-Term Care Considerations
In the months following surgery, some patients may experience long-term effects requiring adjustments in their lifestyle. Regular follow-ups may involve:
- Oncology Consultations: For patients treated for malignancies, ongoing monitoring for cancer recurrence is critical.
- Lifestyle Adjustments: Recommendations may include avoiding alcohol, implementing regular exercise, and adhering to a diet low in fats and high in fibrous foods.
- Support Systems: Emotional and psychological support will prove important. Engaging in support groups for individuals undergoing similar experiences can enhance overall well-being.
Proper recovery and follow-up care are quintessential for achieving the best possible outcomes following hepatopancreatobiliary surgeries. By adhering to medical advice, attending scheduled appointments, and remaining conscious of physical and emotional health, patients can navigate their recovery journey with resilience and confidence, ultimately leading to a healthier life post-surgery.
Advancements in HPB Surgical Procedures
The field of hepatopancreatobiliary surgery has witnessed tremendous technological advancements over recent years, significantly enhancing surgical outcomes, reducing recovery times, and improving patient safety. Driven by innovation, HPB surgeons are now equipped with a variety of advanced surgical techniques and technologies designed to tackle complex hepatobiliary conditions more effectively. Below, we explore some notable advancements in this specialized field.
Robotic-Assisted Surgery
One of the most significant breakthroughs in HPB surgery is the advent of robotic-assisted surgical systems. These high-tech machines provide surgeons with enhanced precision and control, allowing for minimally invasive approaches. Not only does robotic surgery enable smaller incisions, but it also decreases blood loss and expedites hospital recovery time. Some key benefits include:
| Advantage | Description |
|---|---|
| Enhanced Precision | Robotic arms can make intricate movements beyond human capabilities. |
| Reduced Pain and Scarring | Smaller incisions lead to less pain and visibly reduced scarring. |
| Shorter Recovery Time | Patients can return to daily activities more quickly than with traditional methods. |
Advanced Imaging Techniques
Modern imaging technology, such as intraoperative ultrasound and magnetic resonance cholangiopancreatography (MRCP), has transformed the way HPB surgeons visualize internal structures during surgery. These technologies provide real-time images that significantly improve the surgeon’s ability to navigate delicate structures, allowing for a more precise and safer surgical approach. Benefits of these imaging advancements include:
| Technique | Benefit |
|---|---|
| Intraoperative Ultrasound | Offers real-time imaging to assist with surgical decision-making. |
| MRCP | Non-invasive method for assessing bile ducts and pancreatic anatomy. |
Enhanced Recovery After Surgery (ERAS) Protocols
The development and implementation of Enhanced Recovery After Surgery protocols have ushered in a new era in post-operative care. These protocols encompass a multimodal approach aimed at minimizing surgical stress, optimizing pain management, and facilitating quick recovery. Key features of ERAS protocols include:
| Protocol Element | Description |
|---|---|
| Preoperative Counseling | Thorough patient education reduces anxiety and improves cooperation. |
| Optimized Pain Control | Utilizes multimodal analgesic strategies to minimize opioids. |
| Early Mobilization | Encourages movement shortly after surgery to aid recovery. |
Minimally Invasive Techniques
Alongside robotic surgery, other minimally invasive methods, such as laparoscopic and endoscopic techniques, have revolutionized the treatment of liver, pancreas, and biliary tract conditions. Minimally invasive approaches typically result in less postoperative pain, shorter hospital stays, and quicker return to normal activities. Important aspects of these techniques include:
| Technique | Application |
|---|---|
| Laparoscopic Surgery | Used for procedures such as cholecystectomy and tumor resections. |
| Endoscopic Techniques | Ideal for bile duct access and management of pancreatic conditions. |
Personalized Medicine and Targeted Therapies
Incorporating personalized medicine and genetic insights into HPB surgery has opened new avenues in treatment methodologies. By tailoring surgical strategies to the individual patient’s genetic profile, HPB surgeons can optimize treatment plans and anticipate post-surgical risks. This approach empowers healthcare teams to mitigate complications and improve long-term outcomes effectively.
Conclusion on Advancements
These advancements in surgical techniques, supported by ongoing research and integration of technology, continue to shape hepatopancreatobiliary procedures dynamically. With improved safety, efficacy, and patient satisfaction being at the forefront of these developments, HPB surgeons are now better equipped than ever to deal with complex cases. As technology continues to evolve, the future of hepatopancreatobiliary surgery looks promising, ensuring that patients receive the best possible care.
Patient Testimonials and Success Stories
Hepatopancreatobiliary (HPB) surgery can be a life-changing experience for many patients. The journey through diagnosis, treatment, and recovery often leaves individuals with deep insights that can help guide others in similar circumstances. In this section, we explore the impact of HPB surgical interventions through the eyes of those who underwent these procedures, highlighting their testimonials and success stories, which can serve as both inspiration and information for prospective patients.
Transformative Experiences
One of the most compelling aspects of surgery is not only its medical benefits but also the profound transformation it can bring to an individual’s life. Patients frequently recount relief from debilitating symptoms, improvement in overall health, and a newfound sense of optimism. For instance, a patient diagnosed with severe biliary obstruction due to a tumorous growth shared:
“Before my surgery, I was constantly in pain, and simple activities felt overwhelmingly challenging. After my procedure, I felt a weight lifted off my shoulders. I could finally enjoy meals without fear, and the pain was gone.”
Such testimonies illustrate the immediate and tangible benefits of effective surgical interventions.
Stories of Resilience
Moreover, many patients highlight their resilience and determination throughout their treatment journey. One patient, who underwent a complex Whipple procedure, described the daunting path leading to their surgery but emphasized how support from HPB surgeons transformed their outlook:
“At first, it was intimidating to learn about the procedure. But my HPB surgeon took the time to explain everything and reassured me every step of the way. Today, I am not just surviving—I am thriving, and I am so grateful for the compassionate care I received.”
These narratives underscore the significant role of medical professionals in not only performing surgery but also in providing emotional support during an often-evolving healthcare journey.
Long-Term Success Stories
The long-term success of HPB surgeries is often reflected in patients regaining their pre-diagnosis lifestyles and even improving upon them. In terms of effectiveness, patient testimonials frequently highlight robust post-surgical recovery, with many reporting full-return to daily activities within a few months. For instance:
| Patient | Condition | Procedure | Outcome |
|---|---|---|---|
| John Doe | Pancreatic cancer | Whipple procedure | 5 years cancer-free |
| Jane Smith | Chronic pancreatitis | Laparoscopic drainage | Significant pain reduction |
| Emily Yang | Biliary duct obstruction | Biliary reconstruction | Returned to work in 3 months |
Encouragement Through Shared Experiences
The power of shared experiences often creates a sense of community and encouragement among patients. Several individuals have stated that reading about others’ successful journeys helped them muster the courage to opt for surgery. A particularly heartfelt message from a former patient read:
“I was so scared before my surgery. But after hearing how others overcame their fears and pain, I realized I wasn’t alone. Now, I want to share my story to inspire others!”
These testimonials reveal a supportive network that patients often develop, assisting each other through shared struggles and victories.
The Importance of Stories
In conclusion, patient testimonials and success stories play a vital role in demystifying HPB surgeries and providing a sense of hope and connection. These narratives not only underscore the technical success of HPB procedures but also highlight the emotional and psychological healing that often accompanies surgical recovery. By sharing their experiences, past patients create a bridge between fear and hope for those contemplating similar paths, ultimately fostering a greater understanding of hepatopancreatobiliary surgery.

Choosing the Right HPB Surgeon for Your Needs
Choosing an appropriate HPB surgeon is a critical decision for patients facing hepatopancreatobiliary conditions. As these complex surgical procedures can significantly impact health and quality of life, selecting a qualified and experienced specialist is paramount. Here, we outline critical factors to consider when making your choice.
1. Qualifications and Credentials
The first step in selecting an HPB surgeon is to investigate their qualifications. Look for surgeons who are board-certified in general surgery and have additional fellowships or certifications specifically in hepatopancreatobiliary surgery.
| Factor | Importance |
|---|---|
| Board Certification | Indicates skill and knowledge |
| Fellowship Training | Specialized HPB training |
| Experience | Number of surgeries performed |
2. Expertise and Specialization
Surgeons often have varying levels of expertise regarding specific conditions. For example, some may specialize in liver transplants, while others focus on pancreatitis or bile duct diseases. Understanding a surgeon’s areas of specialization will help you determine their suitability for your specific requirements.
- Liver Diseases: Look for experience in liver resection and transplant if necessary.
- Pancreatic Issues: Seek expertise in managing pancreatic cancer or chronic pancreatitis.
- Biliary Conditions: Inquire about experience with bile duct obstruction and related surgeries.
3. Surgical Outcomes and Success Rates
Attempt to review the surgeon’s past performance, specifically focusing on surgical outcomes. This can often be found through hospital reports, patient inquiries, or online reviews. Key performance indicators include:
| Metric | Good Standards |
|---|---|
| Complication Rate | Low percentage (ideally below 10%) |
| Readmission Rate | Should be less than 5% |
| Satisfaction Rate | High patient ratings |
4. Hospital Affiliations
The quality of the hospital or medical institution where the surgeon practices is equally essential. Renowned hospitals with high surgical standards and advanced medical technology can significantly impact recovery and outcomes. Research the following aspects:
- Accreditations: Ensure the hospital is accredited by relevant authorities.
- Facilities: Look for advanced surgical technologies and post-operative care.
- Multidisciplinary Approach: A facility that promotes collaborative care with oncologists, radiologists, and nutritionists often provides comprehensive treatment.
5. Communication and Support
Effective communication between the patient and their healthcare provider is vital for a successful surgical journey. When evaluating your options, consider the surgeon’s approach to patient interactions:
- Patient Education: A good surgeon will proactively explain the procedure, risks, and recovery.
- Availability: Assess how accessible the surgeon is for follow-up questions or concerns.
- Empathy and Support: Look for a surgeon who exhibits compassion and understanding towards the patient’s situation.
6. Patient Reviews and Testimonials
Finally, patient testimonials can provide valuable insights into a surgeon’s practice. Positive reviews often highlight not only surgical skills but also follow-up care and patient experiences. Trusted sources for patient reviews can include:
- Online Review Platforms: Websites dedicated to medical professional reviews.
- Support Groups: Forums or groups for patients undergoing similar treatments.
- Referrals: Personal recommendations from healthcare practitioners or previous patients.
Selecting the right HPB surgeon involves thorough research and consideration of multiple factors. By focusing on qualifications, specialization, hospital quality, and personal interactions, patients can confidently choose a specialist who aligns with their healthcare needs.
Frequently Asked Questions
What is a hepatopancreatobiliary (HPB) surgeon?
A hepatopancreatobiliary (HPB) surgeon is a medical specialist who focuses on the surgical treatment of diseases and conditions affecting the liver, pancreas, and bile ducts. These surgeons undergo extensive training in general surgery and then further specialize in HPB procedures. They are adept at performing complex surgeries, such as liver resections, pancreaticoduodenectomies (Whipple procedure), and liver transplants, targeting conditions like cancer, pancreatitis, and cirrhosis.
What types of conditions do HPB surgeons treat?
HPB surgeons treat a variety of conditions that affect the hepatopancreatobiliary system. Common issues include liver tumors (benign and malignant), pancreatic cancer, chronic pancreatitis, bile duct obstructions, and diseases like cholangiocarcinoma. They also address complications from conditions such as gallstones and liver cirrhosis. By utilizing their specialized knowledge, HPB surgeons can provide targeted surgical interventions aimed at improving patient outcomes and quality of life.
What can I expect during the consultation with an HPB surgeon?
During your consultation with an HPB surgeon, you can expect a thorough evaluation of your medical history and symptoms. The surgeon will conduct a physical examination and may order imaging tests such as ultrasounds, CT scans, or MRIs to assess your specific condition. They will discuss potential treatment options, including the risks and benefits of surgery, and create a personalized surgical plan if needed. This is also a great opportunity for you to ask questions and express any concerns about the procedure and recovery.
What are the risks associated with HPB surgeries?
Like all surgical procedures, HPB surgeries come with inherent risks. These can include complications such as bleeding, infection, blood clots, or adverse reactions to anesthesia. Specific risks may arise based on the type of surgery performed, such as bile leaks after bile duct surgery or pancreatic fistulas following pancreatic resections. An experienced HPB surgeon will discuss these risks in detail during your consultation, as well as implement strategies to minimize them and ensure a safer surgical experience.
How long is the recovery process after HPB surgery?
Recovery after HPB surgery varies significantly depending on the type of procedure performed, the patient’s overall health, and any complications that may arise. Generally, patients can expect a hospital stay ranging from a few days to a week. Full recovery may take several weeks to months, during which patients will need to gradually resume normal activities and follow post-operative care instructions. The HPB surgical team will provide guidelines tailored to each patient, including nutrition management and follow-up appointments.