Lip reconstruction plays a crucial role in restoring not just the physical appearance of the lips, but also their essential function. Whether due to congenital defects, trauma, or surgical removal of cancerous tissues, lip issues can significantly impact an individual’s ability to speak, eat, and express emotions. In this blog post, we will explore the multifaceted aspects of lip reconstruction, including common causes of defects, various techniques employed, and the vital role of tissue grafting. Furthermore, we will discuss postoperative care, potential complications, and the profound psychosocial impacts these procedures can have on patients. Join us as we delve into inspiring success stories and case studies that highlight the transformative power of effective lip reconstruction.
Understanding Lip Reconstruction
Lip reconstruction refers to a collection of surgical procedures aimed at restoring both the form and functionality of the lips. This specialized area within reconstructive surgery encompasses various techniques, tailored to meet individual needs based on the type and severity of the lip defect. Lip anatomy is complex and encompasses not just aesthetic parameters, but also critical functions such as speech, eating, and emotional expression. As such, understanding the intricacies of this surgical field is essential for both patients and healthcare professionals.
Key Components of Lip Anatomy
To comprehend the scope of lip reconstruction, it is crucial to have a solid grasp of the anatomy involved. The primary components of the lips include:
| Component | Description |
|---|---|
| Vermilion | The reddish-colored area of the lips, rich in blood vessels. |
| Philtrum | The vertical groove that runs from the nose to the middle of the upper lip. |
| Cupid’s Bow | The prominent, curved shape of the upper lip. |
| Mucosa | The inner lining of the lips, which is sensitive and moist. |
| Skin | The outer layer providing protection and structure. |
Importance of Function and Aesthetics
Restoring aesthetics is often one of the most immediate concerns for individuals considering lip reconstruction. A well-contoured lip not only enhances facial beauty but also plays a key role in social interactions. However, functional aspects should not be overlooked. The ability to eat, speak, and express oneself emotionally can dramatically improve quality of life. Both these elements must be balanced, as dysfunction often leads to psychological distress even when aesthetic goals are met.
Indications for Lip Reconstruction
Several factors might necessitate such procedures, ranging from congenital anomalies to traumatic injuries. The following are common indications:
| Indication | Description |
|---|---|
| Cleft lip/palate | A congenital defect that may hinder both form and function. |
| Trauma | Injury from accidents or dog bites can result in significant lip defects. |
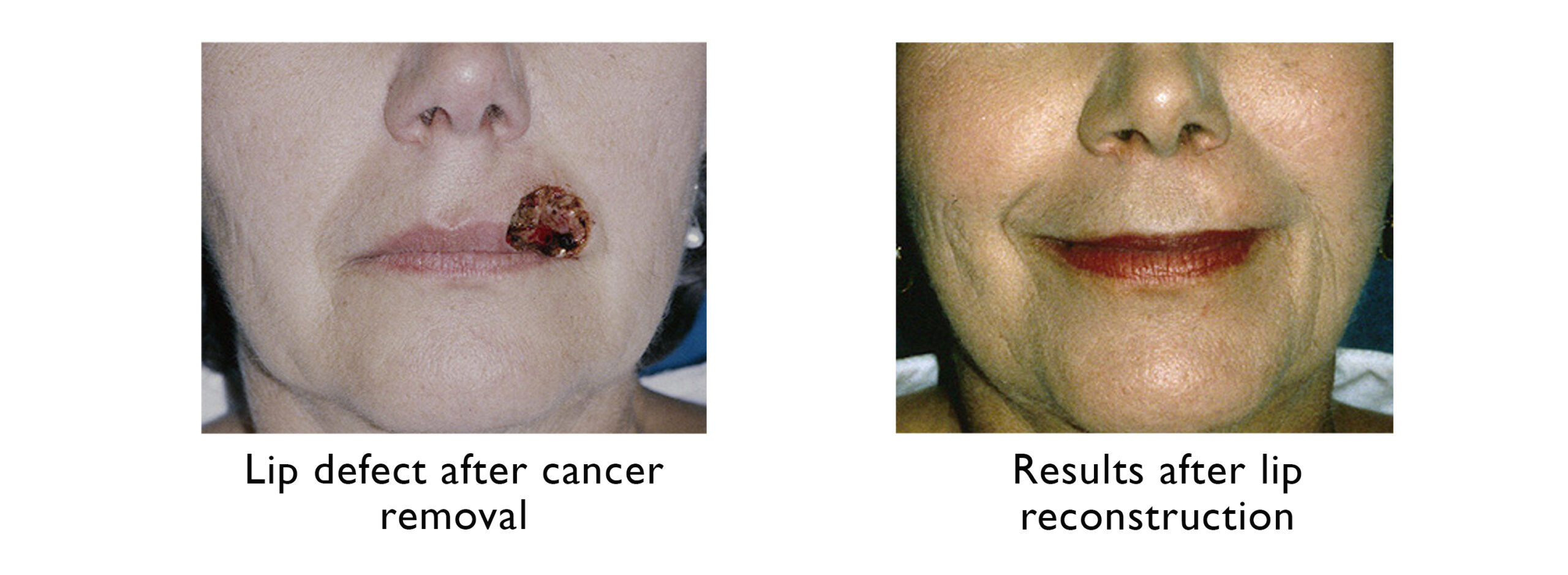
| Tumor removal | Surgical excision of tumors can lead to loss of lip tissue. |
| Burn injuries | Severe burns can cause scarring and deformities in the lip area. |
| Age-related changes | Natural aging can lead to volume loss and changes in lip structure. |
The Role of a Multidisciplinary Team
Effective lip reconstruction often involves a team-oriented approach, including plastic surgeons, speech therapists, and psychologists. Each professional contributes to the overall treatment plan to ensure the best possible outcomes for the patient. This collaborative ethos helps address both the physical and emotional ramifications of lip defects.
The Process of Lip Reconstruction
Understanding the overall process of lip reconstruction is vital for prospective patients. Initial assessments typically include a comprehensive evaluation of the defect, a discussion of patient expectations, and the risks involved in surgical procedures. This step is crucial for formulating an individualized surgical plan that is responsive to both the anatomical and functional needs of the patient.
In summary, a well-rounded understanding of lip reconstruction lays the groundwork for informed decisions regarding treatment options. This specialized area of reconstructive surgery not only aims to achieve aesthetic excellence but also restores vital functionalities that significantly enhance an individual’s quality of life. By appreciating the complexity of this field, patients can embark on their reconstructive journey with greater confidence and clarity.

The Importance of Lip Function and Aesthetics
Lips serve as one of the most expressive and functional parts of the human face. They not only contribute to a person’s aesthetic appeal but also play vital roles in essential activities such as speaking, eating, and facial expressions. Understanding the importance of lip function and aesthetics can help underline the necessity of addressing any defects that may arise due to congenital conditions, trauma, or surgical interventions.
Functional Significance of Lips
Lips are integral to various functions, and when they are compromised, daily life can be significantly affected. Here are some of the primary functions of lips:
| Function | Description |
|---|---|
| Speech | Lips articulate sounds and are essential for phonetics, impacting clarity. |
| Eating | They serve a crucial role in the mechanics of eating and swallowing food. |
| Facial Expressions | Lips help convey emotions, enhancing non-verbal communication. |
| Sensation | Lips are rich in nerve endings, providing sensitivity and tactile feedback. |
Loss of normal lip functionality can lead to considerable challenges. Individuals may struggle with communicating effectively, resulting in frustration and social withdrawal. Furthermore, difficulties in eating may lead to nutritional imbalances, which compound the problems associated with lip defects.
Aesthetic Relevance of Lips
From an aesthetic perspective, lips play a primary role in shaping facial attractiveness. Symmetry, fullness, and color all contribute to a person’s facial identity. When imperfections occur—such as clefts, scars, or injuries—the impact can extend beyond physical appearance, affecting self-esteem and how individuals relate to others. Key aspects of lip aesthetics include:
| Aesthetic Aspect | Description |
|---|---|
| Symmetry | Harmonious lips create a balanced appearance that enhances beauty. |
| Proportions | Full, well-defined lips typically conform to societal standards of attractiveness. |
| Texture and Color | Smooth, evenly pigmented lips are often considered more appealing. |
Unbalanced or abnormally shaped lips can draw attention away from other positive qualities, influencing social interactions and self-image. Society often places significant emphasis on the aesthetic value of lips, which can lead to feelings of inadequacy when perfection is not achieved.
Interconnection Between Function and Aesthetics
It is essential to highlight how functionality and aesthetics are interconnected. For instance, an individual with a reconstructed lip that appears perfectly symmetrical may still experience challenges in speech or eating if functional repair does not accompany aesthetic improvements. Thus, the goals of lip reconstruction should prioritize addressing these simultaneous concerns.
Patients undergoing reconstruction often cite improved confidence and participation in social interactions post-surgery. Successful rehabilitation restores not just the appearance of the lips but their full functional capabilities, allowing individuals to reclaim their voices, experiences, and enjoyment of food.
In summary, the importance of lip functionality and aesthetics cannot be overstated. Both aspects significantly contribute to an individual’s quality of life, self-esteem, and social interactions, necessitating a comprehensive approach to lip reconstruction. As advancements in medical techniques evolve, enhancing both functional and aesthetic outcomes becomes increasingly achievable, offering renewed hope for individuals faced with lip defects.
Common Causes of Lip Defects
Lip defects can emerge from a variety of sources, each often causing both functional and aesthetic challenges. Understanding the common causes of these issues is fundamental for effective intervention and reconstruction strategies. Below is a detailed exploration of these sources, ensuring a comprehensive grasp of their implications.
Congenital Defects
Congenital defects are conditions present at birth, significantly impacting the lips’ structure and function. One of the most prevalent congenital anomalies is cleft lip, which occurs when the tissue forming the lip doesn’t fully come together during fetal development. Here are some key points regarding congenital defects:
| Type of Defect | Description |
|---|---|
| Cleft Lip | A gap or fissure in the upper lip, which can be unilateral or bilateral. |
| Cleft Palate | A split in the roof of the mouth that can accompany a cleft lip. |
| Microform Cleft Lip | A subtle form of cleft lip that may not require surgical correction but can affect aesthetics. |
These conditions can lead to difficulties with feeding, speaking, and hearing, necessitating early intervention for optimal outcomes.
Traumatic Injuries
Traumatic injuries to the lips can arise from various situations, including accidents, dog bites, or physical altercations. The degree of damage may range from minor lacerations to significant tissue loss. The following table summarizes different types of traumatic injuries:
| Type of Trauma | Effect on Lips |
|---|---|
| Lacerations | Cuts that can cause bleeding and pain; often require stitches for closure. |
| Avulsions | Partial or complete tearing away of tissue from the lip; may necessitate grafting procedures. |
| Burns | Can result from heat, chemicals, or radiation, often leading to scarring and functional impairment. |
Effective lip reconstruction after trauma is critical to restore not just the aesthetic appearance but also vital functions such as eating and speaking.
Surgical Complications
Surgeries involving the facial region may inadvertently lead to lip defects. For example, oncologic surgeries aimed at removing tumors can compromise healthy tissue. This can lead to defects that require subsequent reconstructive procedures. Key surgical complications include:
| Type of Complication | Characteristics |
|---|---|
| Scar Formation | Fibrous tissue may distort natural lip contours, affecting both appearance and function. |
| Infection | Poses a risk during and after surgery, which can complicate healing and lead to tissue loss. |
| Necrosis | Death of tissue due to disrupted blood supply, necessitating further reconstructive efforts. |
Addressing these complications is essential to ensure satisfactory restoration outcomes.
Medical Conditions
Certain medical conditions can also contribute to lip defects. For instance, autoimmune disorders such as lupus may cause lesions or ulcers on the lips, leading to functional impairments. Additionally, skin cancers, if left untreated, may require surgical intervention that alters lip structure. Below are some common medical conditions that can affect lip integrity:
| Condition | Impact on Lips |
|---|---|
| Lupus | Can cause swelling, lesions, or ulcers in the oral region. |
| Squamous Cell Carcinoma | May lead to tissue loss requiring surgical intervention. |
| Allergies | Can trigger swelling and inflammation, impacting lip appearance. |
Understanding these medical influences is key to approaching lip reconstruction with a comprehensive, multifaceted strategy.
Conclusion
Comprehending the common causes of lip defects is vital for patients and medical professionals alike. This awareness lays the groundwork for effective treatment planning, ultimately facilitating the restoration of both form and function. By addressing these diverse causes, a more tailored and efficacious approach to lip reconstruction can be developed, leading to improved patient outcomes.
Assessment and Planning for Lip Reconstruction
Assessment and planning are critical steps in ensuring the success of any lip reconstruction procedure. This phase not only sets the stage for the surgical intervention but also equips the medical team with the necessary information to achieve the best possible outcomes for both function and aesthetics. An effective assessment is composed of several key components, including a thorough medical history review, a detailed physical examination, imaging studies when necessary, and careful consideration of the patient’s goals and expectations. Understanding these aspects is crucial for developing a comprehensive reconstruction plan tailored to the individual needs of each patient.
Key Components of Assessment
The assessment process can be broken down into several fundamental components that guide the planning of the reconstruction. These include:
| Component | Description |
|---|---|
| Medical History | A detailed review helps identify any pre-existing conditions, allergies, or medications that may impede the surgical process or affect healing. |
| Physical Examination | Careful evaluation of the lips and surrounding tissues assesses the type and extent of the defect, providing crucial information for determining the most suitable surgical techniques. |
| Diagnostic Imaging | Depending on the nature of the lip defect, imaging studies such as CT or MRI scans may be performed to evaluate the underlying bone structure or soft tissue. |
| Functional Assessment | This involves determining the patient’s ability to perform essential functions like eating, speaking, and controlling saliva, helping to prioritize restoration of functionality. |
| Aesthetic Goals | Discussions with the patient regarding their aesthetic desires guide the surgical plan to align with the patient’s expectations while ensuring realistic outcomes. |
Developing a Comprehensive Plan
Once the assessment is complete, the next step involves creating a strategic surgical plan that considers both functional and cosmetic objectives. This plan typically includes:
- Surgical Technique Selection: Depending on the individual circumstances—whether it’s a cleft lip, trauma, or cancer resection—different techniques such as local flaps, free tissue transfer, or implants may be utilized. The choice is guided by the extent of tissue loss and facial structure.
- Timeline and Phases: Some reconstruction procedures can occur in stages. For complex cases, the plan may be designed to begin with initial tissue expansion or volume restoration, followed by subsequent surgeries aimed at refining aesthetics.
- Involvement of a Multidisciplinary Team: A successful lip reconstruction plan often involves collaboration among various specialists, including plastic surgeons, speech therapists, and orthodontists when required. This multidisciplinary approach enhances overall outcomes by addressing the multiple facets of the lip function and aesthetic restoration.
Patient Education and Informed Consent
An integral part of the assessment and planning phase is educating the patient about the procedure, expected outcomes, and potential risks. This process generally covers:
- Preoperative Instructions: Guidelines on avoiding blood thinners, smoking cessation, and dietary recommendations help optimize the patient’s condition prior to surgery.
- Expectation Management: Discussing realistic expectations related to the healing process, including potential scarring and recovery timelines, is essential to align patient goals with achievable results.
- Informed Consent: Securing informed consent ensures that the patient is fully aware of the procedure, its inherent risks, benefits, and alternatives, thus facilitating empowered decision-making.
In summary, the assessment and planning phase of lip reconstruction is a vital foundation that relies on meticulous evaluation and strategic foresight. By focusing on both functional and aesthetic aspects while engaging the patient in the decision-making process, healthcare providers can effectively enhance the likelihood of successful outcomes.

Techniques Used in Lip Reconstruction
When it comes to restoring both the function and aesthetics of the lips, a variety of surgical techniques have been developed. The choice of method often depends on the specific condition being treated, the extent of tissue loss, and the desired cosmetic outcome. Understanding these techniques can provide valuable insights into the journey toward lip restoration.
Common Techniques for Lip Reconstruction
1. Primary Closure
This technique is often employed for small defects. It involves reuniting the skin and underlying tissues after a surgical excision. The closure is performed in such a way to maintain a natural appearance and preserve lip function.
2. Local Flaps
For moderate-sized defects, local flap techniques are frequently utilized. This method involves moving nearby tissue to cover the defect while maintaining its blood supply. Specifically, the following types of local flaps are commonly used:
- Z-Plasty: This technique utilizes triangular flaps to reposition scar lines and create a more aesthetically pleasing contour. It helps camouflage scars and makes them less noticeable.
- Advancement Flaps: This technique allows for tissue to be pulled forward from adjacent areas, which is particularly useful when reconstructing the lip’s vermilion border.
3. Free Tissue Transfer
For larger defects or those resulting from traumatic injuries, free tissue transfer techniques become necessary. Surgeons may use tissue from other areas of the body (such as the forearm or thigh) to reconstruct the lip. This involves microvascular surgery to reattach blood vessels, which ensures that the transplanted tissue survives.
4. Composite Grafts
In some cases, a combination of skin and mucosal tissue may be grafted to recreate the lip structure. These composite grafts help in achieving a more natural appearance by layering different types of tissues, which mimic the original lip’s texture.
The Role of Surgical Techniques
The methods applied during lip reconstruction aim not just to repair physical appearance but also to restore functionality. Each surgical technique can be further tailored to address specific needs discussed in the table below:
| Technique | Ideal For | Aesthetic Benefits | Functional Benefits |
|---|---|---|---|
| Primary Closure | Small, clean defects | Minimal scarring | Quick recovery of lip movement |
| Local Flaps | Moderate-sized defects | Natural growth of surrounding tissue | Improved lip shape and function |
| Free Tissue Transfer | Large defects or traumatic injuries | Enhanced contour and volume | Full restoration of sensation and movement |
| Composite Grafts | Complex deformities | Multi-dimensional texture | Regenerated lip contour and functionality |
Key Considerations
In determining which technique to use, plastic surgeons must carefully assess factors such as the location, size, and depth of the defect along with the patient’s overall health and lifestyle. The chosen method should aim for the best possible balance between aesthetic desires and functional needs.
Additionally, advancements in surgical technology and techniques are continuously improving the outcomes of lip reconstruction, leading to less invasive procedures and quicker recovery times. With the right approach, patients can achieve not only a return to normalcy but also an enhanced sense of self-confidence and well-being through this transformative process.
Postoperative Care and Recovery
Postoperative care and recovery after undergoing procedures aimed at lip reconstruction represent critical phases in the journey toward restoring both function and aesthetics of the lips. This stage encompasses numerous essential actions that can significantly influence healing, minimize discomfort, and enhance final outcomes. Properly addressing these components ensures that the objective of the surgical intervention is realized effectively. Below is a detailed overview of the postoperative care and recovery process.
Key Components of Postoperative Care
A structured postoperative care plan typically includes:
| Component | Description |
|---|---|
| Pain Management | Effective pain control techniques, including prescribed medications and alternatives like ice packs, help alleviate discomfort. Assessing pain levels regularly is crucial. |
| Wound Care | Keeping the surgical site clean and dry is vital. Specific instructions may involve using gentle cleansers and applying topical antibiotics, if recommended. |
| Swelling Management | Swelling commonly occurs in the initial days post-surgery. Ice packs, applied intermittently, aid in reducing inflammation and promote comfort. |
| Activity Restrictions | Patients are usually advised to avoid strenuous activities and heavy lifting for a specified duration, allowing the body to heal without added strain. |
| Nutritional Support | A balanced diet rich in vitamins and proteins can assist in the healing process. Emphasizing the consumption of soft foods may also help reduce strain on the lips. |
Typical Recovery Timeline
Understanding the recovery timeline fosters better preparedness, allowing patients to anticipate healing stages:
| Day | Expected Changes |
|---|---|
| 1-3 | Initial swelling and bruising. Pain may peak during this period. |
| 4-7 | Gradual reduction of swelling; stitches, if used, may be removed. |
| 1-2 weeks | Significant improvement in pain; lip functionality begins to stabilize. Swelling may persist but will gradually diminish. |
| 1 month | Most aesthetic improvements become evident; the patient may resume normal activities with caution. |
| 3 months | Final results visible; ongoing softening and refinement of lip contours. |
| 6 months + | Long-term care, continued assessments, and monitoring for complete healing and resolution of aesthetics. |
Important Instructions for Patients
Adhering to postoperative instructions is indispensable in achieving optimal results. Key postoperative care instructions typically include:
- Avoidance of Smoking: Smoking can significantly impair healing and increase complications. Patients are strongly discouraged from smoking for at least a few weeks post-surgery.
- Regular Follow-Up Appointments: Scheduled visits with the surgeon facilitate tracking recovery progress and addressing any concerns promptly.
- Limitation on Oral Activity: Caution is advised against excessive talking and eating hard foods, which can stress the surgical site.
- Sun Protection: Protecting healing lips from sun exposure by using lip balms with SPF or covering the area is crucial to prevent discoloration.
Long-Term Considerations
Long after the initial recovery, it’s vital to maintain lip health and aesthetics. This commitment may involve regular evaluations, the use of moisturizing products, and protection from environmental factors. Engaging in a healthy lifestyle with an emphasis on hydration, nutrition, and skin care will also support ongoing wellness.
Each step taken during the postoperative care and recovery phases contributes to a seamless transition to full functionality and aesthetic appeal. By understanding and implementing these critical components, individuals can ensure that their lip reconstruction journey is filled with optimism and positive results.
Potential Complications and Risks
Lip reconstruction, while offering promising results in restoring both function and aesthetics, does carry certain risks and potential complications. Understanding these challenges is crucial for anyone considering such procedures. By being aware of the possible outcomes, individuals can make informed decisions and anticipate the recovery journey.
Common Complications in Lip Reconstruction
| Complication | Description | Possible Causes |
|---|---|---|
| Infection | Bacterial invasion at the surgical site, potentially leading to delayed healing. | Poor hygiene, non-compliance with postoperative care, or underlying health issues. |
| Hematoma | Accumulation of blood outside blood vessels, causing swelling and discomfort. | Trauma to blood vessels during surgery. |
| Scarring | Formation of fibrous tissue, potentially altering the appearance of the lip. | Surgical technique and individual healing response. |
| Skin Flap Failure | Insufficient blood supply to the transplanted tissue, leading to tissue necrosis. | Poor vascularization or underlying conditions like diabetes. |
| Asymmetry | Uneven appearance of the lips post-surgery, affecting aesthetics. | Surgical technique, healing, and the natural anatomy of the lips. |
| Sensory Changes | Alteration or loss of sensation in the lip area. | Nerve damage during the procedure. |
| Difficulties in Speech or Eating | Temporary or persistent issues with lip function, impacting communication or nutrition. | Unanticipated changes to lip structure post-reconstruction. |
Factors Influencing Complications
Several factors can contribute to the occurrence of complications in lip reconstruction. Patient-related factors might include age, overall health, and any pre-existing medical conditions like diabetes or autoimmune disorders, all of which could complicate healing. Surgeon skill and experience also play a significant role. Therefore, selecting a qualified and experienced surgeon is paramount to mitigating risks effectively.
Preventive Measures
To minimize the possibility of complications, certain preventive measures can be taken:
- Preoperative Assessment: Comprehensive health evaluations must be conducted to identify any underlying conditions that may affect recovery.
- Adherence to Postoperative Care: Following the surgeon’s instructions regarding care and hygiene is critical. This includes avoiding strenuous activities and adhering to medication regimens to prevent infections.
- Regular Follow-up Visits: These visits allow medical professionals to monitor recovery and address any arising issues promptly.
- Safe Surgical Environment: Ensuring that the procedure is performed in a certified surgical facility helps reduce risks associated with sterile technique and professional care.
Long-Term Considerations
Potential complications may not solely affect the immediate postoperative phase; some individuals may experience long-term implications, such as persistent scarring or functional difficulties. It’s essential to consider these when assessing the overall benefit of the reconstruction against the risks involved. Furthermore, discussing these potential issues with the healthcare team can provide clarity and assist in setting realistic expectations.
Psychological Impact
Experiencing complications still further emphasizes the psychosocial aspects of lip reconstruction. Individuals may undergo feelings of frustration or disappointment, which can impact their mental well-being. Open communication with mental health professionals, along with support groups, can be beneficial in navigating these feelings.
In summary, while the journey through lip reconstruction can be fraught with potential complications, understanding these risks builds a foundation for making informed decisions and ultimately leads to better outcomes.
Psychosocial Impact of Lip Reconstruction
Lip reconstruction often goes beyond the restoration of physical appearance and function; it plays a significant role in the psychosocial well-being of individuals. Aesthetic changes resulting from congenital issues, trauma, or surgical procedures can profoundly affect someone’s self-esteem, social interactions, and overall mental health. This section delves into the multifaceted psychosocial effects of lip reconstruction and highlights the importance of psychological support throughout the journey.
Emotional Well-Being Post-Reconstruction
Undergoing lip reconstruction can evoke a range of emotions. Many individuals report feelings of anxiety or apprehension before the procedure, particularly regarding their post-operative appearance. However, the satisfaction and joy experienced after achieving a more balanced and functional lip structure can significantly enhance emotional well-being. Here’s a closer look at the emotional outcomes:
| Emotional Aspect | Pre-Reconstruction | Post-Reconstruction |
|---|---|---|
| Self-Esteem | Often lower due to visible defects | Typically improved with enhanced appearance |
| Body Image | Negative perception of one’s own image | More positive body image and confidence |
| Anxiety Levels | High, related to appearance and social interactions | Reduced anxiety as individuals feel more accepted |
| Happiness | May experience sadness or frustration | Increased happiness due to improved functionality and aesthetics |
Social Interactions and Relationships
Aesthetic imperfections can lead to social withdrawal or strained relationships. Individuals may feel self-conscious, leading them to avoid social gatherings or intimate situations, fearing judgment or ridicule. Following successful lip reconstruction, many report positive changes in their social lives.
Research shows that individuals who undergo these procedures often experience:
- Greater Engagement: Individuals may feel more inclined to participate in social activities, resulting in improved relationships and opportunities for socialization.
- Enhanced Communication: Properly reconstructed lips enable clearer speech, which reduces misunderstandings and fosters better connections with others.
The Role of Support Systems
The importance of a robust support system cannot be overstated in the context of lip reconstruction. Friends, family, and counselors play critical roles in the emotional and psychological recovery process. Patients often benefit from engaging in support groups, which provide a safe space to share experiences, fears, and triumphs. This interplay of support can lead to numerous positive outcomes:
- Understanding: Support networks help individuals feel less isolated and understood during their journey.
- Motivation: Encouragement from close ones can foster resilience and a positive outlook towards recovery.
- Sharing Experiences: Interacting with those who have undergone similar experiences can provide motivation and realistic expectations for the outcome.
Long-Term Psychological Benefits
The long-term benefits of lip reconstruction often extend well beyond the immediate satisfaction of improved aesthetics. Many studies have indicated sustained improvements in mental health, suggesting that even years after the procedure, individuals report enhanced quality of life and emotional well-being.
- Increased Self-Confidence: Many individuals find that their self-belief significantly improves, enabling them to pursue personal and professional goals with newfound vigor.
- Emotional Resilience: Overcoming the challenges associated with recovery can foster greater resilience and coping skills that benefit multiple aspects of life.
The psychosocial impact of lip reconstruction is profound and multifaceted. By restoring not only the aesthetic appearance but also enhancing emotional and social aspects of life, individuals can achieve a fulfilling reintegration into their personal, social, and professional environments. Consequently, ensuring access to psychological support and community connections can greatly enhance recovery outcomes, cementing the significance of a holistic approach in the field of reconstructive surgery.
Success Stories and Case Studies
Lip reconstruction plays a crucial role in transforming the lives of individuals facing challenges due to congenital defects, trauma, or disease. Numerous success stories highlight the significant impacts of these surgical interventions, reflecting both aesthetic restoration and functional improvement. This section delves into inspirational accounts of patients who have undergone lip reconstruction, demonstrating the profound changes these procedures can facilitate.
Journey of Transformation: Real-Life Stories
1. Juan’s Story: Rebuilding After Trauma
Juan, a 35-year-old construction worker, faced a life-altering accident that resulted in extensive damage to his upper lip. Prior to the reconstructive surgery, Juan experienced challenges with eating and speaking, leading to social withdrawal and emotional distress. After a comprehensive assessment, a surgical team developed a customized plan involving tissue grafting and flap techniques to repair the damaged area.
Post-operation, Juan described his newfound ability to articulate words clearly and enjoy meals without discomfort. His dramatic transformation not only restored his appearance but also revitalized his confidence, enabling him to return to work and actively engage with friends and family.
| Aspect | Before Reconstruction | After Reconstruction |
|---|---|---|
| Eating | Difficulty, pain, limited choices | Ability to enjoy varied meals |
| Speaking | Slurred, hard to understand | Clear articulation |
| Emotional Health | Social withdrawal, low self-esteem | Increased confidence, social re-engagement |
2. Sarah’s Journey: From Birth Defect to Empowerment
Sarah, born with a congenital condition known as a cleft lip and palate, underwent multiple procedures throughout her childhood. As an adult, she sought further reconstruction to enhance the aesthetics of her lips and improve functionality. Her medical team adopted a phased approach, carefully planning each surgery to minimize scarring and optimize results.
Following her final reconstruction, Sarah was overjoyed with her enhanced appearance and newfound ability to smile freely. She has actively shared her experience, becoming a voice for others with similar conditions, and has emphasized how reconstruction improved not just her physical characteristics, but her overall self-image.
| Aspect | Childhood Challenges | Adulthood Post-Reconstruction |
|---|---|---|
| Lip Appearance | Visible asymmetry | Balanced aesthetic, pleasing smile |
| Functional Issues | Difficulty in feeding and speaking | Normalized eating and speaking abilities |
| Self-Image | Low confidence | Empowered and inspired to help others |
The Broader Impact
The impact of lip reconstruction extends beyond mere physical alteration. Patients often experience a surge in self-esteem and emotional well-being, which significantly alters their interpersonal relationships and overall quality of life. The stories of individuals like Juan and Sarah illustrate that successful reconstructive surgery transcends aesthetics, offering a renewed sense of purpose and dignity.
Conclusion of the Impact Narrative
These narratives not only showcase the technical proficiency of reconstructive surgeons but also highlight the holistic benefits of these life-changing procedures. As advancements in techniques and technology continue to evolve, the potential for transformative healing remains boundless, promising brighter futures for many patients.
Frequently Asked Questions
What is lip reconstruction?
Lip reconstruction is a surgical procedure designed to restore the shape, function, and aesthetics of the lips after injury, trauma, or congenital defects. This procedure is crucial for individuals who have suffered from lip deformities, whether due to accidents, cancer surgeries, or other medical conditions. The surgery involves techniques that aim to rebuild the lip structure, improve symmetry, restore fullness, and enhance overall appearance, ensuring that the patient regains both functionality for speaking and eating, as well as a natural look.
What are the common reasons for undergoing lip reconstruction?
People may undergo lip reconstruction for a variety of reasons. These include congenital deformities such as cleft lip, trauma from accidents or burns, surgical removal of tumors, and infections. Additionally, some individuals seek lip reconstruction to correct aesthetic issues caused by the aging process or to improve the overall symmetry of the face. The goal is to restore not only the visual appeal but also the functional capabilities of the lips, enhancing the patient’s quality of life.
What is the recovery process like after lip reconstruction surgery?
The recovery process after lip reconstruction can vary based on the complexity of the surgery and individual health factors. Typically, patients can expect some swelling, bruising, and discomfort in the first few days post-surgery. Pain relief medications are often prescribed to manage discomfort. Most patients are advised to stick to a soft diet and avoid strenuous activities for a few weeks. Follow-up visits with the surgeon will be necessary to monitor healing and ensure optimal results. Full recovery, including final aesthetic results, may take several months.
Are there any risks associated with lip reconstruction?
As with any surgical procedure, lip reconstruction carries potential risks. These may include infection, excessive bleeding, scarring, and adverse reactions to anesthesia. Additionally, there is a possibility of dissatisfaction with the aesthetic results, which could require further revision surgery. It is crucial for patients to discuss these risks with their surgeon during the consultation, as well as to have realistic expectations regarding the outcomes of the procedure.
How can I prepare for a lip reconstruction procedure?
Preparing for lip reconstruction involves several important steps. First, patients should undergo a thorough consultation with their surgeon to discuss their medical history, the specific procedure, and expected outcomes. It is advisable to avoid blood-thinning medications and smoking for a few weeks prior to surgery to minimize complications. Patients should also plan for post-operative care, including arranging for assistance during the initial recovery days, and preparing a comfortable recovery environment at home.