In a world where body image and self-esteem play significant roles in overall well-being, nipple reconstruction surgery stands out as a transformative option for many individuals seeking to restore both form and confidence following trauma or surgery. This procedure not only helps in enhancing physical appearance but also addresses the emotional aspects that accompany breast surgery. Throughout this post, we will explore the ins and outs of nipple reconstruction, from understanding the surgical techniques to the psychological benefits it offers, ensuring you have all the information needed to make informed decisions. Join us as we dive into the various facets of this empowering journey, shedding light on patient stories, aftercare tips, and essential considerations for choosing a qualified surgeon.
What is Nipple Reconstruction Surgery?
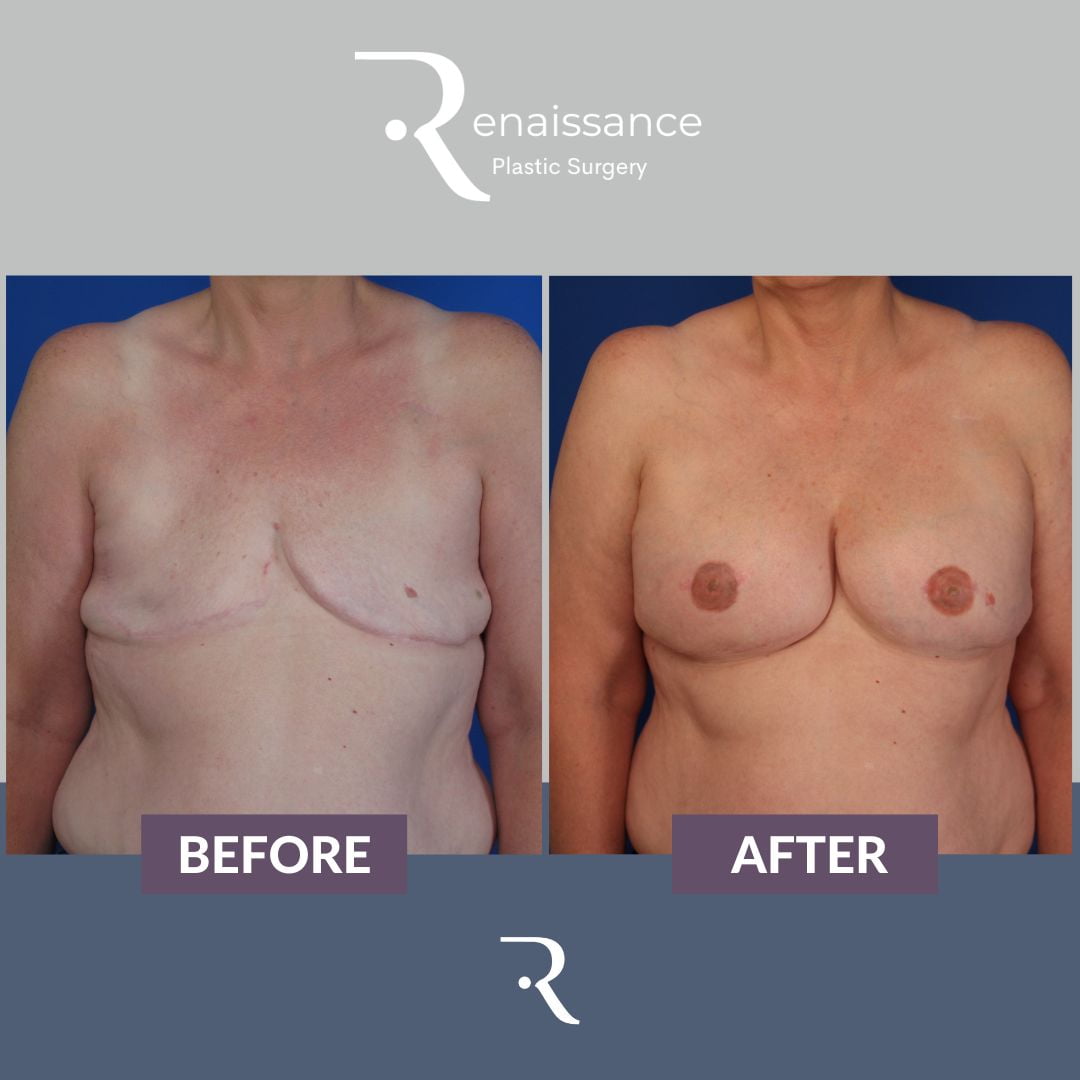
Nipple reconstruction is a specialized surgical procedure designed to recreate the appearance of the nipple and areola after mastectomy or other breast surgeries. This transformative intervention not only addresses the physical changes that accompany breast reconstruction but also plays a pivotal role in restoring psychological well-being and confidence among individuals who have undergone significant alterations to their breast tissue.
The Purpose of the Procedure
The primary goal of this surgical process is to help patients regain a more natural look following the loss of the nipple. Aside from aesthetic appeal, it emphasizes the importance of enhancing the overall body image and emotional recovery. By reconstructing a nipple, patients often experience a profound sense of closure and completeness in their journey towards healing.
Types of Reconstruction Techniques
There are several innovative techniques utilized in this type of surgery, each tailored to the individual’s unique needs and health conditions. Here are some prevalent methods:
| Technique | Description |
|---|---|
| Local Flap Technique | Tissue is taken from surrounding skin and is reshaped to form a new nipple. |
| Skin Graft | A thin layer of skin is harvested from other body areas, like the thigh or abdomen, to form a nipple. |
| Tattooing | Involves applying pigment to simulate an areola appearance, usually performed after the primary reconstruction. |
Timing of the Surgery
The timing of the procedure can vary widely depending on a patient’s individual situation. For some, the reconstruction occurs concurrently with breast reconstruction, while others may choose to wait until they have physically and emotionally healed. The timing is typically discussed in great detail with the surgical team, who will consider various factors like healing from prior surgeries, overall health, and personal preferences.
The Nipple Reconstruction Journey
A consultation with a qualified surgeon is the first step in this rewarding journey. During this consultation, patients are educated about the various techniques, options, and expected outcomes. It serves as an opportunity to discuss personal goals, ask questions, and understand the implications of the surgery.
Before the procedure, a thorough medical assessment is performed, ensuring that patients are in optimal condition for surgery. During the surgery itself, local or general anesthesia may be employed, depending on the complexity of the technique used and the surgeon’s discretion.
Patients can anticipate not only a physical transformation but also an emotional rejuvenation as they embrace their new image. The process often culminates in a renewed sense of identity and empowerment, as they take significant steps in reclaiming their lives post-surgery.
This procedure should not be viewed solely as a cosmetic enhancement; rather, it is a crucial component of the overall journey of recovery. It plays an essential role in the holistic approach to healing, helping individuals feel more comfortable and confident in their bodies again.

Indications for Nipple Reconstruction
Nipple reconstruction surgery is primarily performed to restore the appearance of the nipple and areola after mastectomy, trauma, or congenital absence. Understanding the specific indications for this surgery can help individuals make informed decisions about their options for body restoration and enhancement of overall self-esteem. Below is a detailed overview of the primary indications for undergoing nipple reconstruction surgery.
1. Mastectomy Recovery
Many women (and some men) undergo mastectomy as part of breast cancer treatment. During this procedure, the breast tissue, which may include the nipple and areola, is removed to eliminate cancer cells. Consequently, many patients seek nipple reconstruction as a subsequent step to restore the natural appearance of their breast. This surgical intervention can significantly aid in emotional recovery, helping patients regain a sense of normalcy.
2. Trauma to the Breast Area
Injuries or traumatic events can lead to significant changes in the breast structure, including the loss or alteration of the nipple. This could occur as a result of accidents, burns, or other medical emergencies. Individuals who experience such trauma may consider nipple reconstruction to improve the aesthetic appearance of their chest and restore their physical integrity.
3. Congenital Absence
Some individuals are born with a congenital absence of the nipple or areola, a condition known as congenital amastia or nipple hypoplasia. For those affected, nipple reconstruction surgery is a viable option that can enhance their overall appearance, boost confidence, and allow them to embrace their body fully.
4. Changes Due to Aging
As individuals age, the natural changes in skin elasticity and breast tissue can result in significant alterations in breast shape, texture, and appearance, leading to a retracted or flat nipple. Nipple reconstruction can be a straightforward way to address these physical changes, revitalizing not just appearance but also personal confidence.
5. Gender-affirming Procedures
Additionally, transgender individuals undergoing gender-affirming surgery may seek nipple reconstruction as part of their transition process. This can be critical in aligning their physical presentation with their gender identity, thus boosting confidence and ensuring that their outward appearance reflects their inner self.
| Indication | Description |
|---|---|
| Mastectomy Recovery | Restoration after breast cancer surgery for emotional well-being. |
| Trauma to the Breast Area | Repairing appearance following injuries or accidents. |
| Congenital Absence | Addressing absence of nipple due to congenital factors. |
| Changes Due to Aging | Restoring aesthetics of nipples affected by aging. |
| Gender-affirming Procedures | Fulfilling the physical aspects of transitioning. |
6. Symmetrical Breast Appearance
For individuals who have undergone unilateral mastectomy or breast surgeries that affect one side, nipple reconstruction can also serve as a way to achieve symmetry. Having a more balanced appearance can improve the overall aesthetic outcome and boost self-esteem.
Emotional and Psychological Benefits
Beyond the physical components, the emotional and psychological indications for pursuing nipple reconstruction are substantial. Many individuals report feeling incomplete or disconnected from their bodies post-procedure or due to congenital factors. Therefore, undergoing nipple reconstruction can provide significant advantages that extend well beyond mere appearance, ultimately leading to improved mental health and emotional well-being.
In summary, nipple reconstruction surgery can address a wide range of indications from medical conditions to personal choices and transitions. By understanding these indications, individuals can empower themselves to explore options that boost both confidence and quality of life.
The Surgical Techniques Used in Nipple Reconstruction
Nipple reconstruction surgery is a personalized procedure that aims not only to restore the physical appearance of the nipple but also to enhance the overall self-image of individuals who have undergone mastectomy or experienced trauma. The surgical techniques employed can vary based on the patient’s anatomy, preferences, and specific circumstances surrounding their reconstruction.
Common Surgical Techniques
There are several primary methodologies used for performing nipple reconstruction surgery. Below is a comparison of the most widely adopted techniques:
| Technique | Description | Advantages | Disadvantages |
|---|---|---|---|
| Pedicle Flap Technique | Utilizes skin and tissue from the surrounding area, maintaining blood flow. This flap is shaped into a nipple. | Natural appearance; good blood supply. | Potential for longer surgery time; may affect surrounding tissue. |
| Skin Graft Method | Involves taking a graft of skin from another body area, typically the abdomen or thigh, to create a new nipple. | Simple and effective; versatile use of tissue. | May not blend perfectly with breast skin; possible color variations. |
| Tissue Expansion | Involves stretching the skin before placing an implant to create a nipple mound. | Provides volume; can achieve desired projection. | Requires multiple procedures; may lead to discomfort during expansion. |
| 3D Tattooing Technique | While not a surgical procedure, this technique can be used post-reconstruction to add depth and color. | Offers realistic appearance; no surgical risks. | Depending on artist’s skill; not an actual physical reconstruction. |
Detailed Overview of Each Technique
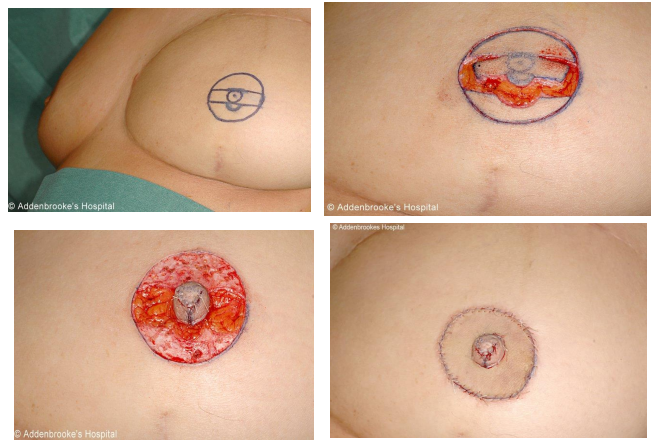
Pedicle Flap Technique
This method involves surgically creating a nipple using a flap of skin and tissue that remains attached to the underlying artery. The surgeon carefully sculpts this tissue to form a new nipple, which maintains its blood supply. This technique is favored for its ability to create a very natural look and feel.
Skin Graft Method
In this technique, a small section of skin is removed from a donor site—often the abdomen or thigh. The skin is then shaped and stitched to resemble a nipple. This method is particularly useful for patients with insufficient skin at the mastectomy site. Although straightforward, successful color and texture match can sometimes be challenging.
Tissue Expansion
Tissue expansion is a gradual process that involves inserting a tissue expander beneath the skin that will form the nipple. Over a few months, the expander is filled with saline to stretch the skin slowly. Once the desired amount of skin has been expanded, the expander is replaced with an implant. This method is beneficial for those desiring more projection and volume in their reconstructed nipple.
3D Tattooing Technique
After surgical options have been explored, many individuals opt for 3D nipple tattoos. Highly skilled tattoo artists use specialized techniques to create the illusion of depth and texture on the skin, enhancing the appearance of the reconstructed nipple. This non-surgical option is often performed in conjunction with surgical methods to achieve a more complete and aesthetically appealing result.
Factors Influencing Technique Selection
Choosing the appropriate technique for nipple reconstruction surgery depends on multiple factors, including:
- Patient Health: Overall health and the presence of underlying medical conditions can influence the choice of technique.
- Personal Preference: Patients may have specific desires regarding the appearance of the nipple.
- Surgeon’s Expertise: The surgeon’s experience and familiarity with different techniques can play a vital role in the outcomes and patient satisfaction.
In conclusion, the surgical techniques for nipple reconstruction are diverse and tailored to meet individual needs. Understanding these methods can help patients make informed decisions that align with their goals for restoration and self-confidence.
The Role of 3D Nipple Tattoos in the Process
In the journey to restoring form and confidence after breast reconstruction, the art of 3D nipple tattoos plays a pivotal role. These innovative tattoos offer an aesthetic solution that complements surgical interventions, creating the illusion of natural-looking nipples. But how do these tattoos enhance the overall process of nipple reconstruction surgery? Let’s explore their significance, technique, and the emotional benefits they provide.
Enhancing Aesthetic Outcomes
One of the primary benefits of 3D nipple tattoos is their ability to create the visual appearance of depth and dimension. Unlike traditional tattooing methods, which may only replicate the surface features of a natural nipple, 3D tattoos employ advanced techniques to create realistic shadows and highlights. This results in a lifelike, three-dimensional effect that can significantly enhance the overall outcome of nipple reconstruction—a crucial aspect for those seeking completeness and balance in their breast profile.
Key Components of 3D Nipple Tattoos
| Component | Description |
|---|---|
| Technique | Use of shading and color gradients to create depth |
| Materials | Medical-grade pigments designed to minimize allergic reactions |
| Preparation | Skin assessed for suitability; specific guidelines for pre-procedure care |
| Aftercare | Tips for caring for the tattoo to maintain vibrancy and prevent infection |
The Tattoo Process
The process of applying a 3D nipple tattoo generally occurs after surgical healing is complete, often several months post-procedure. Here’s a brief overview of the steps involved:
- Initial Consultation: During the first meeting, the tattoo artist will discuss the individual’s desires, color palettes, and specific anatomical features.
- Design Creation: Customized designs are drawn, taking into account the shape and alignment of the breast area post-reconstruction.
- Tattoo Application: The application is performed using sterile equipment and precise techniques to achieve the desired 3D effect. The artist may utilize various hand techniques that allow for fine detail, ensuring authenticity.
- Healing and Aftercare: Patients are provided with care instructions to promote healing, including keeping the area clean and avoiding sun exposure.
Emotional and Psychological Aspects
The psychological impact of a well-executed 3D nipple tattoo can be profound. For many individuals, achieving a realistic nipple design is not just about aesthetics; it symbolizes reclaiming their body and, ultimately, their identities. This rejuvenating effect can significantly boost self-esteem and body image, offering a tremendous sense of closure after the trauma of surgeries related to breast cancer or congenital anomalies.
Moreover, personal stories of transformation often highlight the immense satisfaction felt when seeing themselves fully restored, both physically and emotionally. Patients frequently report feeling more confident in intimate situations and public settings, leading to a more positive outlook on life.
Professional Training and Expertise
It is essential that individuals seeking 3D nipple tattoos choose qualified professionals. Artists should have specialized training in medical tattooing and experience in creating aesthetically pleasing results that resonate with the patient’s personal vision. Collaboration with plastic surgeons can further enhance outcomes, ensuring that the tattoo complements any surgical interventions.
In summary, 3D nipple tattoos provide an invaluable enhancement to the nipple reconstruction surgery process, significantly contributing to the aesthetic and emotional well-being of individuals reclaiming their identity. By utilizing advanced techniques and prioritizing personalized care, these tattoos help conclude a journey marked by resilience and transformation, paving the way for greater confidence and self-acceptance.

Recovery Process and Aftercare
Recovery from nipple reconstruction surgery is a crucial phase that plays a significant role in the overall success of the procedure. Understanding the necessary aftercare can not only facilitate the healing process but also enhance the satisfaction with the results. Here’s an in-depth look at what patients can expect during the recovery period and how they can take care of themselves post-surgery.
Immediate Post-Operative Care
Right after the surgery, patients are monitored in a recovery area. Here are some vital components of immediate post-operative care:
| Aspect | Details |
|---|---|
| Duration in Recovery Room | Typically 1-2 hours, until stable |
| Monitoring Vital Signs | Heart rate, blood pressure, and oxygen saturation |
| Medication | Pain relief and anti-nausea medications may be administered |
| Dressings | Sterile dressings will be applied to the surgical site |
Early Recovery Phase (1-2 Weeks)
During the first weeks after surgery, it’s essential to follow care instructions meticulously to avoid complications. Some key recommendations include:
- Rest and Relaxation:
- Limiting physical activities is crucial. Patients should avoid heavy lifting and strenuous exercise.
- Wound Care:
- Keeping the area clean and dry is vital. Regularly inspect the dressings for any signs of infection, such as increased redness or discharge.
- Follow-Up Appointments:
- Attending scheduled follow-ups enables the surgeon to assess healing and address any concerns.
Mid- to Late Recovery Phase (2-6 Weeks)
As the recovery progresses, patients will notice improved comfort levels and reduced swelling. However, continued care is essential:
| Care Recommendations | Details |
|---|---|
| Gradual Activity Resumption | Light activities can generally be resumed after 2 weeks. |
| Continued Monitoring | Regularly check for changes in swelling or sensitivity. |
| Skin Care | Moisturizing the area can assist healing once cleared by the surgeon. |
Long-Term Aftercare (6 Weeks and Beyond)
After the initial healing period, several ongoing care practices contribute to long-term results and emotional well-being:
- Physical Sensation:
- Patients may experience changes in sensitivity over time. It is critical to be patient as nerve regrowth can take months.
- Psychological Support:
- Emotional healing may take longer than physical recovery. Seeking counseling or joining support groups can be beneficial.
- Sun Protection:
- The reconstructed area may be sensitive to sun exposure. Wearing sunblock is recommended to prevent hyperpigmentation.
Emotional Adjustment
The journey does not end with physical recovery. Psychological well-being plays a pivotal role in the healing process:
- Self-Image: Many patients report a boost in self-esteem post-reconstruction. However, it’s essential to give oneself time to adjust to the new appearance.
- Support Systems: Engaging with loved ones or joining resources can help in managing feelings and expectations during recovery.
In summary, the recovery process following nipple reconstruction surgery requires a comprehensive understanding of care practices, monitoring, and emotional support. Patients who adhere to these guidelines often report heightened satisfaction with their results and an improved quality of life.
Potential Risks and Complications
When considering nipple reconstruction surgery, it is essential to be aware of the potential risks and complications that may arise. Although many patients experience successful outcomes with little to no complications, understanding these risks can assist in making an informed decision. Here, we will examine the various kinds of risks involved, ranging from minor inconveniences to more serious medical issues.
Common Risks
| Risk | Description |
|---|---|
| Infection | Infection at the surgical site can lead to pain, redness, and swelling. Serious infections may require antibiotics or further intervention. |
| Scarring | Like any surgical procedure, scarring is a possibility. Patients will have different healing patterns, and some may develop more noticeable scars. |
| Changes in Sensation | Some individuals report altered sensation around the nipple area, including numbness, tingling, or heightened sensitivity. These changes may be temporary or permanent. |
Less Common Complications
Though less common, specific complications should still be highlighted:
| Complication | Description |
|---|---|
| Asymmetry | In some cases, the reconstructed nipple may not match the other nipple in size, shape, or color. This may necessitate additional procedures to achieve symmetry. |
| Poor Healing | Some patients might experience delayed wound healing, which can lead to further complications and may prolong recovery. |
| Necrosis | In rare instances, tissue can die due to insufficient blood supply, leading to the need for revision surgery. |
Managing Risks
Before undergoing nipple reconstruction surgery, it is crucial to have open discussions with your healthcare provider about your medical history, current medications, and any underlying health conditions. These factors can significantly influence your risks.
Preoperative Assessment
A thorough preoperative assessment can help identify:
- Previous surgeries: Any prior procedures in the area could increase scarring or alter blood flow.
- Medical conditions: Conditions like diabetes or autoimmune disorders can complicate recovery.
The surgical team will discuss with you about:
- Smoking status: Smoking can impair healing and lead to complications; cessation before surgery can reduce risks significantly.
- Medication management: Certain medications, especially blood thinners, may need to be adjusted or stopped prior to surgery to minimize bleeding risks.
Postoperative Monitoring
After the surgery, close attention should be paid to signs of infection or other complications. Patients should be educated on the following symptoms:
- Increased redness or swelling
- Fever
- Changes in drainage from the surgical site
- Persistent pain or discomfort
Immediate communication with your healthcare provider can be invaluable if any of these symptoms arise.
By being aware of the potential risks and complications associated with nipple reconstruction surgery, patients can take proactive steps to ensure a smooth surgical journey. Through thorough preparation and diligent aftercare, many complications can be effectively managed or avoided, allowing patients to focus on their recovery and the restoration of their confidence.
Psychological Impact of Nipple Reconstruction
The journey through breast cancer treatment can be physically demanding and emotionally challenging, leaving many individuals feeling a profound sense of loss. Nipple reconstruction surgery emerges as a beacon of hope for many, contributing not only to physical restoration but also to psychological healing. Understanding the psychological impact of nipple reconstruction surgery is important for patients, caregivers, and healthcare providers alike.
Emotional Restoration
The emotional turmoil following a mastectomy or breast surgery often includes feelings of grief, loss of femininity, and a diminished self-image. Nipple reconstruction surgery can play a critical role in reversing some of these psychological effects. The ability to restore a more natural appearance to the breast can enhance self-esteem and body image, allowing individuals to reclaim their sense of identity and femininity.
In many cases, patients report an increase in their overall happiness and confidence post-surgery. This restoration translates to daily life, impacting interpersonal relationships and sexual intimacy positively, which are crucial facets of the human experience.
Community and Support
Reconstructive procedures, including nipple reconstruction surgery, often lead patients to seek connection within support groups and communities. Sharing experiences with others who have undergone similar procedures amplifies feelings of support and understanding. These interactions can be invaluable.
The psychological benefits of feeling connected and understood frequently contribute to enhanced emotional resilience. Patients often report having a renewed sense of purpose and motivation by communicating with others on the same journey.
Coping Strategies and Mental Health
Psychological support is vital throughout the recovery process. Patients are encouraged to engage in various coping strategies such as:
| Coping Strategy | Description |
|---|---|
| Counseling | Professional therapy can help address any lingering grief or anxiety. |
| Support Groups | Engaging with peers who have experienced similar challenges can enhance healing. |
| Mindfulness Practices | Techniques such as meditation or yoga can foster a positive mindset, aiding emotional recovery. |
| Art Therapy | Creative expression can be a powerful conduit for processing emotions related to body image. |
| Physical Activity | Regular exercise has been shown to improve mood and promote positive body image. |
Recognition and Acceptance
Patients often navigate a complex journey toward acceptance after nipple reconstruction surgery. Recognizing the changes to the body and adapting to the new appearance can take time. Some individuals struggle with feelings of incompleteness or dissatisfaction, even post-reconstruction.
Education about the realistic outcomes of nipple reconstruction can aid in managing these expectations. Open conversations with healthcare providers about potential results and psychological implications should occur prior to surgery.
Long-Term Considerations
The psychological impact of nipple reconstruction surgery tends to evolve over time. Initial feelings of joy may shift as patients come to terms with their new reality. Continuous support, both psychological and social, is crucial to ensure that patients maintain a healthy outlook on their body image and self-worth.
Regular follow-ups with mental health professionals can aid in addressing any emerging concerns over time. Ultimately, the goal is for patients to find strength and empowerment through their journey, embodying a sense of wholeness post-reconstruction.
Nipple reconstruction surgery is not merely a procedure; it’s a significant step toward emotional healing and restoring personal agency in the post-cancer experience.
Patient Stories and Testimonials
Patient stories and testimonials are invaluable in the realm of nipple reconstruction surgery, offering real-life insights into the experiences and emotions associated with the procedure. These narratives not only highlight the physical transformations but also underscore the psychological healing and renewed sense of confidence that many individuals experience post-surgery. Here, we delve into a variety of personal accounts that illuminate the impact of this transformative surgery.
Empowering Journeys: Real-Life Experiences
Many individuals who undergo nipple reconstruction surgery have faced significant emotional and physical challenges. For instance, a 35-year-old breast cancer survivor, Sarah, described her experience as a reclaiming of her identity. “After my mastectomy, I felt like I lost a part of myself. The surgery helped me feel whole again,” she recounted. This emotional restoration is a common theme among patients, emphasizing the surgery’s role not just in aesthetics, but also in enhancing self-esteem and mental well-being.
Mark, a 45-year-old male who underwent reconstruction following gender-affirming surgery, shared, “The reconstruction gave me the confidence to embrace my body. I finally feel like I can present myself to the world fully.” Stories like Mark’s are essential in recognizing how nipple reconstruction can cater to a diverse group, helping individuals transition in ways that align with their identity and sense of self.
Testimonials Highlighting the Process
- Emily’s Transformation: A Path of Resilience
- Operation: Emily underwent nipple reconstruction a year after her mastectomy.
- Post-Op Experience: “The first look in the mirror was overwhelming. It was a moment where I felt I was finally home in my body.”
- Psychological Outcome: Emily mentioned feeling empowered to wear what she wanted without the anxiety of showing scars.
- Tom’s Journey to Acceptance
- Motivation: After surviving breast cancer, Tom wanted to complete his journey of recovery.
- Satisfaction: “The moment I saw the final results, I cried tears of joy. It’s like getting a second chance.”
- Community Impact: Tom has since become an advocate, sharing his story to help others facing similar battles.
The Ripple Effect of Positive Experiences
Patients frequently express gratitude not just for the surgery itself, but for the comprehensive care they received. A common sentiment shared among patients is appreciation for their medical team, with many highlighting the importance of emotional support throughout the process. For instance, Jenna said, “The surgeons and nurses took the time to listen to my concerns, making me feel valued. This holistic approach made all the difference.”
In Their Own Words: A Collection of Reflections
| Patient Name | Age | Procedure | Key Takeaway |
|---|---|---|---|
| Sarah | 35 | Nipple Reconstruction | “I reclaimed my identity.” |
| Mark | 45 | Gender-affirming surgery | “I can finally present myself fully.” |
| Emily | 29 | Mastectomy & Reconstruction | “It was a moment of being home in my body.” |
| Tom | 52 | Breast cancer survivor | “It’s like getting a second chance.” |
The stories we encounter reveal an undeniable truth: nipple reconstruction surgery is about more than the physical changes. It profoundly influences lives, inspiring hope and confidence in ways that resonate deeply with both the individuals and their communities. By sharing their journeys, these patients encourage others to take the step toward reclaiming their lives post-surgery, fostering a sense of hope and a supportive network.
How to Choose a Qualified Surgeon
Selecting a qualified surgeon for nipple reconstruction surgery is a pivotal step that significantly impacts the outcome of your procedure. With the emotional and physical aspects linked to this surgery, ensuring that you are in the hands of an experienced and skilled professional is crucial for achieving both aesthetic results and peace of mind. Below are detailed guidelines to assist you in making an informed decision when selecting a surgeon for your nipple reconstruction.
Research Credentials and Specializations
Begin by verifying the surgeon’s educational background and training. Check for board certification in plastic surgery, as this indicates that the surgeon has undergone rigorous training and has met specific professional standards. It’s also beneficial to ascertain if the surgeon specializes in breast reconstruction or aesthetic surgery, as they will have the most relevant experience.
| Criteria | What to Look For |
|---|---|
| Board Certification | Verified by the American Board of Plastic Surgery (ABPS) |
| Surgical Specialization | Focus on breast or reconstructive surgery |
| Experience | Minimum of 5-10 years in the field |
Evaluate Past Work
Reviewing a surgeon’s previous work can provide insight into their capabilities and artistic sensitivity. Look for before-and-after photos of their nipple reconstruction surgeries, which can often be found on their websites or through social media. This visual evidence will help you determine if their results align with what you hope to achieve. You may also inquire about their patient satisfaction rates and seek testimonials.
Consultation Process
The initial consultation is a critical moment in assessing a potential surgeon. This is your opportunity to ask questions, voice concerns, and gauge the surgeon’s approach to patient care. Make sure to address the following points during your consultation:
- Technique and Options: Discuss the various surgical techniques available and understand the pros and cons of each.
- Personalized Plan: A great surgeon will tailor their approach to your individual anatomy and personal desires.
- Post-Op Care: Inquire about the level of post-operative follow-up care you can expect.
Assess Communication and Comfort
Effective communication is key to a successful surgical experience. Throughout the consultation, assess how well the surgeon listens to your needs and how clearly they explain the procedure. Feeling comfortable and confident in your surgeon allows for a collaborative relationship, which is essential for addressing any potential fears or anxieties about the surgery.
Check Reviews and Referrals
Customer reviews and referrals can reveal invaluable information about a surgeon’s reputation. Look for online reviews on platforms like RealSelf and Healthgrades, where previous patients share their experiences. Additionally, asking for referrals from trusted individuals in your support system, or other healthcare professionals, can point you towards reputable surgeons.
Consider Hospital Affiliations
The quality of the hospital where the surgeon operates plays a significant role in your overall surgical experience. Research the surgical facilities affiliated with your chosen surgeon to ensure they are accredited and equipped with necessary resources for safe and effective care.
Financial Considerations
Lastly, it’s essential to understand the financial aspects. Ask the surgeon about their fee structure and whether your insurance will cover any portion of the nipple reconstruction surgery. Clarity on these financial obligations can prevent misunderstandings and help you budget accordingly.
Navigating the journey toward informed decision-making in selecting a qualified surgeon may seem overwhelming, but it is crucial for peace of mind and optimal outcomes. Equip yourself with the right questions and research to ensure a successful reconstructive surgery experience that aligns with your personal goals and expectations.
Insurance Coverage and Financial Considerations
Navigating the financial aspects of nipple reconstruction surgery can be a daunting process. Understanding insurance coverage and other financial implications is crucial for patients contemplating this transformative procedure. This section aims to shed light on the various financial considerations and insurance policies that can impact the cost of surgery.
Understanding Insurance Coverage
One of the foremost concerns for patients is whether health insurance will cover nipple reconstruction surgery. While coverage policies can differ significantly among insurers, many plans are likely to cover the procedure when it is deemed medically necessary. Here are some key points to consider regarding insurance coverage:
| Factors Affecting Coverage | Details |
|---|---|
| Medical Necessity | Coverage is more common if surgery follows a mastectomy or injury. |
| Pre-authorization Requirements | Many insurers require pre-approval; patients must submit relevant documentation. |
| Network Providers | Coverage varies if you use an in-network vs. out-of-network surgeon. |
| Additional Procedures | Some plans may bundle coverage for additional operations like breast reconstructions. |
Financial Considerations
Even if surgery is covered, patients should still prepare for various out-of-pocket expenses. Understanding these costs helps in budgeting effectively:
- Deductibles and Co-pays: Many insurance plans have deductibles—fixed amounts that must be paid before coverage kicks in. Additionally, there may be co-pays for consultations or surgical procedures.
- Surgeon’s Fees: Depending on the surgeon’s experience and location, fees may vary. It’s important for patients to obtain a detailed estimate beforehand.
- Anesthesia and Facility Costs: These expenses can add up quickly. Inquire with your surgical center about additional fees, including anesthesia services or facility charges.
- Follow-up Care: Post-surgical care, including follow-up appointments and therapy, may not always be covered by insurance. Patients should factor in these potential costs.
- Payment Plans: Some surgical centers offer flexible payment plans that allow patients to break down costs over time. Inquire about such options, along with any financing services that may be available.
Additional Resources
To further assist patients, several organizations can help in navigating financial matters related to nipple reconstruction surgery. These resources include:
- Patient Advocacy Groups: Organizations such as the American Society of Plastic Surgeons often provide information on insurance policies and financial assistance.
- Financial Counselors: Many hospitals have financial counselors who can assist patients in understanding their coverage and securing necessary approvals.
- Online Tools: Websites like Healthcare.gov offer comparison tools for different insurance plans, helping patients to choose the most suitable option according to their needs and financial situation.
Conclusion of Financial Thinking
In summary, while financial considerations surrounding nipple reconstruction surgery may seem overwhelming, key factors such as insurance coverage, out-of-pocket expenses, and available resources can streamline the process. Patients are encouraged to thoroughly review their insurance policy, seek detailed cost estimates from their surgeon, and explore available financial assistance programs. These proactive steps will not only enhance the overall experience but also enable patients to focus on their recovery while alleviating financial stress.
Frequently Asked Questions
What is nipple reconstruction surgery?
Nipple reconstruction surgery is a surgical procedure designed to recreate the appearance of a nipple after breast surgery or mastectomy. This procedure can help restore the aesthetic look of the breast, as well as enhance self-esteem and body image for those who have undergone breast cancer treatment or surgery. Various techniques can be used, including local flaps and tattoos, to achieve a realistic appearance.
Who is a suitable candidate for nipple reconstruction surgery?
Ideal candidates for nipple reconstruction surgery are individuals who have had a mastectomy or significant breast surgery that resulted in a loss of the nipple. However, it is crucial that candidates are in good overall health and have realistic expectations for the outcomes of the procedure. A thorough consultation with a qualified plastic surgeon will help determine eligibility based on personal health histories and specific circumstances.
What is the recovery process like after nipple reconstruction surgery?
The recovery process after nipple reconstruction surgery can vary from person to person, but generally, patients can expect some swelling and tenderness for several days. The majority of patients can return to normal activities within one to two weeks; however, it is advisable to avoid strenuous activities for several weeks post-surgery. Follow-up appointments with the surgeon are important to ensure proper healing and to address any concerns during the recovery phase.
Will I be able to feel sensation in my reconstructed nipple?
In many cases, the sensation may not fully return in the reconstructed nipple because the nerves that provide feeling are often removed with the original nipple during mastectomy. However, some patients still report a degree of sensation returning over time, although it can vary significantly from person to person. Discussing expectations regarding sensory outcomes with your surgeon can help in understanding what may be expected after the surgery.
Are there any risks associated with nipple reconstruction surgery?
Like any surgical procedure, nipple reconstruction surgery carries certain risks. These include infection, scarring, dissatisfaction with the cosmetic results, and potential complications related to anesthesia. It is important for individuals considering this surgery to have a detailed conversation with their surgeon about these risks, as well as the potential benefits, to make an informed decision that aligns with their personal health and cosmetic goals.