Are you struggling with excess abdominal skin after significant weight loss or pregnancy? If so, you’re not alone. The journey to achieving a healthier, more confident body often leaves behind unwanted skin that can impact your self-esteem and comfort. In this comprehensive guide, we will explore panniculectomy surgery, a procedure designed to remove this surplus skin and help you regain a smooth silhouette. Throughout this post, you’ll learn about who qualifies for the surgery, what the procedure entails, how to prepare for it, and what to expect during recovery. We will also delve into the potential risks, benefits, and costs involved. Whether you’re contemplating this surgery or simply seeking information, our insights will equip you with the knowledge to make an informed decision about your body and health.
What is Panniculectomy Surgery?
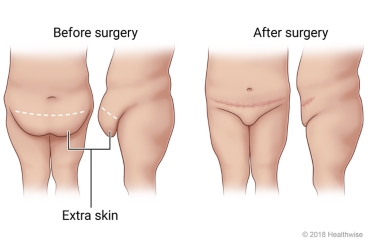
Panniculectomy is a surgical procedure designed to remove excess skin and fat from the lower abdomen, specifically the pannus, which is the sagging abdominal tissue that hangs over the pubic area. This surgery is often sought after significant weight loss, pregnancy, or aging, where the skin loses its elasticity and fails to retract tightly around the abdominal area. Unlike a tummy tuck, which entails tightening of the abdominal muscles, panniculectomy focuses primarily on the removal of the excess skin, thus providing a flatter abdominal contour and minimizing issues related to hygiene or mobility associated with the hanging tissue.
Key Features of Panniculectomy Surgery
Understanding the characteristics of this procedure is essential for potential candidates. Here are some defining aspects:
| Feature | Description |
|---|---|
| Surgical Technique | Performed under general anesthesia, the procedure involves excising excess skin and fat from the abdomen. |
| Incision Site | A horizontal incision is typically made above the pubic area, sometimes extending to the hips. |
| Postoperative Scarring | While the surgery will leave scars, they are generally placed low enough to be concealed by underwear. |
| Hospital Stay | Normally conducted in an outpatient setting, some cases may require a short hospital stay for recovery. |
| Duration | The procedure usually lasts between 2 to 5 hours, depending on the amount of tissue being removed. |
Ideal Candidates for Panniculectomy Surgery
Individuals considering this surgery should evaluate their own situations against certain criteria. Here are factors that determine if someone is a suitable candidate for this operation:
- Weight Stability: Candidates should have achieved a stable weight for at least six months to a year prior to surgery. Fluctuating weight may compromise the results.
- Physical Health: Overall health is vital. Ideal candidates are typically non-smokers with manageable health conditions, as compromised health can increase surgery risks.
- Motivation for Procedure: A strong desire for a better quality of life, often related to physical discomfort caused by excess skin, is essential. Candidates should seek enhancement in their daily activities rather than just aesthetic changes.
- Understanding of the Procedure: It is crucial for candidates to have realistic expectations about the results, potential complications, and the recovery process.
Benefits Beyond Aesthetics
While many individuals pursue panniculectomy for cosmetic reasons, there are additional health-related benefits. These include:
- Improved Hygiene: Removing excess skin can alleviate rashes and skin infections that can occur in skin folds.
- Enhanced Mobility: Patients often report improved mobility and comfort, allowing them to engage in physical activities more freely.
- Increased Self-Esteem: Many find that the change significantly boosts confidence and body image, leading to an overall better quality of life.
In summary, panniculectomy surgery plays a crucial role for those with excess abdominal tissue, offering both physical and emotional benefits. By understanding the procedure, potential candidates can better assess their options and make informed decisions about their health and well-being.

Who is a Suitable Candidate for Panniculectomy?
Panniculectomy is a surgical procedure designed to remove excess skin and tissue, primarily from the abdominal area, typically following significant weight loss or pregnancy. Identifying suitable candidates for this surgery involves a comprehensive evaluation of various physical, emotional, and lifestyle factors. Below is a detailed breakdown of the criteria that help determine if an individual is a good candidate for panniculectomy.
Key Criteria for Suitability
| Criteria | Description |
|---|---|
| Weight Stability | Candidates should maintain a stable weight, generally for at least six months. This stability ensures that the body will not undergo further significant changes post-surgery. |
| Excess Abdominal Skin | Ideal candidates typically have a substantial amount of excess skin that causes discomfort, irritation, or hygiene issues. The presence of a pannus, or a large fold of skin, can sometimes impede daily activities. |
| Overall Health | Individuals should be in good overall health. Pre-existing conditions like heart disease, uncontrolled diabetes, or weakened immune systems can complicate surgery and recovery. |
| Non-Smokers | Candidates are often advised to be non-smokers, as smoking can impair healing and increase the risk of complications. Those who do smoke may be asked to quit for a prescribed period before and after surgery. |
| Realistic Expectations | A suitable candidate should have realistic expectations about the outcome. Understanding that while panniculectomy can significantly enhance appearance and comfort, it is not a weight-loss procedure and will leave some scarring. |
| Psychological Readiness | Emotional readiness is vital. Individuals should be prepared for the transformation that follows the surgery and understand the recovery process. Mental health stability plays a crucial role in post-operative satisfaction. |
| Age Considerations | While there is no strict age limit, the majority of suitable candidates are adults (typically over 18) who have completed their growth and bodily changes, leading to potential eligibility for the procedure. |
Additional Factors to Consider
When determining eligibility for panniculectomy, some individuals should also consider their lifestyle habits, motivations, and support systems. Here are additional factors to evaluate:
- Motivation: Candidates should genuinely seek the surgery for personal reasons rather than to meet someone else’s expectations.
- Financial Readiness: As the procedure is often elective, ensuring financial preparedness is essential. It is advisable to explore insurance coverage, as some policies may vary in terms of covering surgeries related to significant weight loss.
- Physical Activity: Individuals who maintain active lifestyles often experience reduced complications and faster recovery times.
Consultation with a Qualified Physician
A comprehensive consultation with a board-certified plastic surgeon is crucial to determine candidacy accurately. During this visit, the surgeon will assess medical history, perform a physical examination, and discuss any concerns regarding the desired outcome. This dialogue can clarify the procedure’s risks and benefits, assisting individuals in making well-informed decisions.
In summary, suitable candidates for panniculectomy typically possess several key attributes ranging from stable weight and overall health to realistic expectations and emotional readiness. Evaluating these criteria with a healthcare professional is the best approach to determine the appropriateness of this life-enhancing procedure.
Understanding the Procedure of Panniculectomy
Panniculectomy, a surgical procedure primarily aimed at removing excess abdominal skin, is becoming increasingly common among individuals seeking to restore their body’s contours and improve their quality of life. Understanding the nuances of this procedure is crucial for potential candidates who wish to make informed decisions.
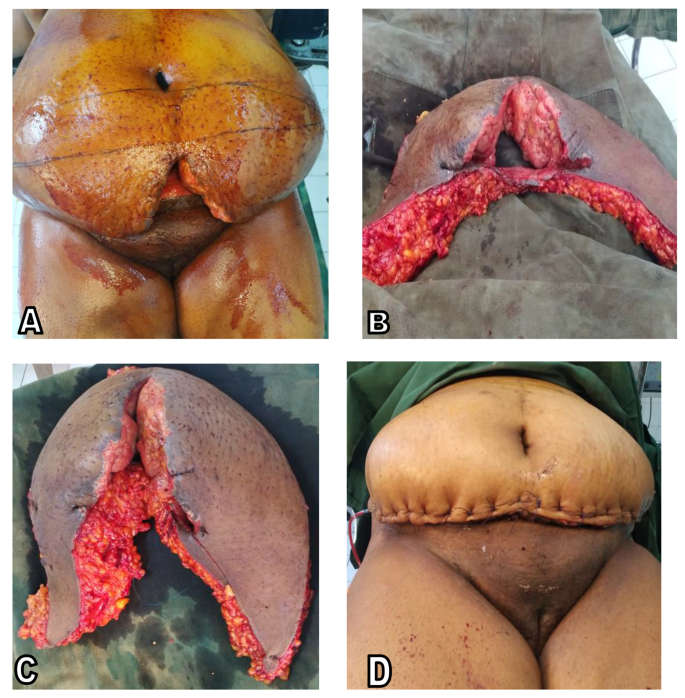
The Surgical Steps Involved
The procedure typically follows a structured approach involving several key steps:
- Preoperative Assessment: This initial phase includes consultations with a board-certified plastic surgeon, who will evaluate the patient’s medical history, perform a physical examination, and discuss realistic outcomes and expectations.
- Anesthesia Administration: Before surgery begins, anesthesia is administered to ensure the patient remains comfortable throughout the operation. Often, general anesthesia is used, allowing the patient to be completely unconscious, although local anesthesia combined with sedation might also be an option based on the specific case.
- Incision Creation: The surgeon then proceeds to make incisions, which usually occur just above the pubic area and may extend around the sides of the abdomen. The design of the incision greatly depends on the individual’s body type and the amount of excess skin present. Below is a comparison of common incision types used in panniculectomy:
Type of Incision Description Indication Horizontal Incision A curved cut above the pubic area, extending to the sides. Mild to moderate excess skin. Extended or Anchor Incision A larger T-shaped incision allowing for more extensive skin removal. Significant excess skin and fat. - Tissue Removal: Once the incisions are in place, the surgeon carefully excises the excess skin and underlying fat. The exact amount removed varies per individual, with the primary goal being to achieve optimal abdominal contour while preserving important structures such as blood vessels and nerves.
- Layered Closure: The incision sites are then closed using advanced techniques that may include sutures or skin adhesives. Surgeons often employ layered closure methods to ensure the wound heals well, minimizes scarring, and creates a flatter abdominal profile.
- Postoperative Monitoring: Once the surgery concludes, patients are typically monitored in a recovery area to ensure no immediate complications arise. Depending on individual conditions, some patients may be discharged on the same day, while others might require an overnight stay for further observation.
What Happens During the Surgery?
The duration of the procedure can vary significantly based on factors such as the extent of skin removal and the patient’s overall health. On average, panniculectomy can last anywhere from two to five hours. Patients will also be connected to intravenous fluids and monitoring equipment to ensure their safety during the entire process.
After the Procedure
As the anesthesia wears off, patients may experience some discomfort in the abdominal region, which is typically manageable with prescribed pain medications. It is crucial to follow post-operative care instructions provided by the surgical team to promote healing and reduce the risk of complications.
In summary, understanding the entire procedure of panniculectomy is essential for anyone considering it. Comprehensive knowledge about the steps involved, the type of incisions used, and what to expect post-surgery can empower patients to discuss their concerns and preferences with their healthcare provider, leading to better overall satisfaction with the outcomes.
Preparing for Panniculectomy Surgery
Preparing for a surgical procedure can be a nerve-wracking experience, and when it comes to panniculectomy, planning ahead is essential to ensure a smooth process. Proper preparation can not only help ease anxiety but can also enhance recovery outcomes. Here, we will explore the significant steps to take as one gears up for this transformative surgery.
Preoperative Consultation
Before undergoing the surgery, individuals will usually have a consultation with their surgeon. During this initial meeting, the following will likely occur:
- Medical History Review: Expect to provide a thorough medical history, including any past surgeries, existing medical conditions, allergies, and medications.
- Physical Examination: The surgeon should perform an examination to assess the abdominal area and discuss the desired outcomes.
- Setting Realistic Expectations: It’s critical to understand what results can realistically be achieved and the limitations of the procedure.
Lifestyle Adjustments
In the weeks leading up to the surgery, certain lifestyle changes can contribute to a smoother recovery:
| Lifestyle Factor | Recommended Action |
|---|---|
| Nutritional Choices | Adopt a healthy eating plan. Focus on lean proteins, whole grains, and plenty of fruits and vegetables to enhance healing. |
| Smoking Cessation | Quit smoking at least four weeks before and after surgery; nicotine can impair blood circulation and slow healing. |
| Alcohol Reduction | Minimize alcohol consumption to maintain good liver function and overall wellness. |
| Hydration | Stay well-hydrated, as fluids help with recovery and skin elasticity. |
Medications and Supplements
A comprehensive discussion regarding medications is crucial. Patients should review their current medications with their surgeon. Specific actions may be necessary:
- Adjusting/Stopping Certain Medications: Blood thinners like aspirin or anticoagulants may need to be discontinued a week before surgery to reduce the risk of bleeding.
- Vitamins and Herbs: Some dietary supplements, such as certain herbs, can interfere with blood clotting; therefore, it is advisable to stop these at least two weeks prior to the procedure.
Day-of-Surgery Preparations
On the day leading up to the surgery, additional preparations will help ensure everything goes smoothly:
- Fasting Instructions: Typically, patients will be advised to refrain from eating or drinking after midnight before the surgery.
- Arranging Transportation: Since sedation is often used during the procedure, it’s necessary to have a responsible adult available to provide transportation home afterward.
- Pre-Surgical Hygiene: Some surgeons may recommend a special antiseptic soap to reduce the risk of infection. Patients are often advised to shower the night before or the morning of the surgery.
Emotional Readiness
Emotional preparation is equally as vital as physical readiness. It is not uncommon to experience a range of emotions leading up to surgery. Here are a few strategies to manage anxiety:
- Educate Yourself: Understand the procedure thoroughly; knowledge can reduce fears of the unknown.
- Support Systems: Lean on family and friends for emotional support. They can assist with travel needs, post-surgery care, and overall encouragement.
- Relaxation Techniques: Practices such as deep breathing, meditation, or yoga can help cut down on stress and foster a sense of calmness.
In summary, adequate preparation is key to navigating panniculectomy surgery efficiently. By tackling these essential aspects, individuals can ensure both their mental and physical state is conducive for the upcoming surgical experience.
What to Expect During Recovery
Recovery from panniculectomy surgery is a crucial phase that greatly influences the overall outcome of the procedure. Understanding what to expect can help patients to prepare both physically and mentally for the healing process. The recovery timeline typically varies from individual to individual, depending on several factors such as overall health, the extent of the surgery, and adherence to post-operative care instructions.
Initial Recovery Phase
Immediately following the surgery, patients are transferred to a recovery room where healthcare professionals closely monitor vital signs such as heart rate and blood pressure. Common experiences during this period may include:
- Pain and Discomfort: It is normal to experience some degree of pain after the procedure. Medications prescribed by the surgeon will help manage this discomfort. Patients are advised to take analgesics regularly to prevent acute pain from setting in.
- Swelling and Bruising: Surgical sites typically swell as part of the body’s natural healing process. Bruising may also occur, which usually resolves within a few weeks.
- Drains and Bandages: Surgical drains may be placed to remove excess fluid that accumulates in the surgical area. These are generally removed a few days post-surgery, depending on the individual’s healing rate.
Early Mobility
Getting moving as soon as feasible is crucial for recovery. Patients are often encouraged to start walking slowly within the first 24 hours post-surgery. Light activity promotes circulation, decreases the risk of blood clots, and can aid in the healing process.
| Activity | Timeline Post-Surgery | Notes |
|---|---|---|
| Walking | 1-2 days | Start with short distances. |
| Light household tasks | 1-2 weeks | Avoid heavy lifting. |
| Driving | 2-4 weeks | When cleared by the surgeon. |
| Return to full activity | 6-8 weeks | Gradual increase as tolerated. |
Long-Term Recovery
The recovery process continues well beyond the initial weeks. Patients generally notice significant changes over several months. Here’s what to expect during the long-term recovery phase:
- Follow-Up Visits: Regular follow-up appointments are essential to monitor the healing process, assess scars, and address any concerns. These typically occur 1-2 weeks after surgery, and then at regular intervals thereafter.
- Scar Management: Scarring is a natural part of the healing process. Patients may need to use silicone gel applications or other treatments prescribed by their surgeon to minimize visible scarring.
- Physical Activity Adjustments: While light physical activity is encouraged, patients should avoid high-impact exercises or activities that strain the abdominal area for at least six weeks after surgery.
Emotional and Psychological Considerations
It’s also vital to prepare for the emotional aspect of recovery. Many patients experience a range of emotions, from excitement about their new appearance to anxiety about their changing bodies. Support from friends, family members, and possibly counseling can aid during this transitional period.
Maintaining a healthy lifestyle with a balanced diet and regular exercise will enhance healing and improve long-term results. Keeping communication open with healthcare providers regarding pain management, emotional concerns, or recovery challenges can facilitate a smoother recovery journey.
Overall, by staying informed and adhering to post-surgical guidelines, patients can significantly enhance their recovery experience following panniculectomy surgery, leading to optimal results and improved quality of life.
Potential Risks and Complications
Panniculectomy is a surgical procedure aimed at removing excess skin from the abdomen, often a result of significant weight loss, pregnancy, or other factors. While many individuals seek this operation for aesthetic and health improvements, it is crucial to understand the potential risks and complications associated with it.
Common Risks of Panniculectomy
As with any surgical intervention, there are inherent risks involved. The common risks associated with this type of surgery include:
| Risk | Description |
|---|---|
| Infection | Surgical site infections can occur, necessitating further treatment and antibiotics. |
| Bleeding | Excessive bleeding may happen during or after the procedure, possibly requiring a blood transfusion. |
| Scarring | Surgical incisions can lead to scarring, which may be permanent depending on the healing process. |
| Fluid Accumulation | Accumulation of seroma (fluid collection) beneath the skin may require drainage. |
| Nerve Damage | Temporary or permanent numbness and changes in sensation can occur in the area treated. |
| Delayed Healing | Certain factors, including smoking and pre-existing conditions, may slow down the healing process. |
Specific Complications That May Arise
Beyond the common risks, specific complications can occur as a result of panniculectomy surgery, including:
| Complication | Potential Impact |
|---|---|
| Wound Separation | The edges of the surgical wound may separate, leading to prolonged healing times. |
| Blood Clots | Deep vein thrombosis (DVT) or pulmonary embolism are serious risks that arise post-surgery, particularly if mobility is limited. |
| Anesthesia Risks | Reactions to anesthesia may occur, particularly in individuals with pre-existing health conditions. |
| Dissatisfaction with Results | Patients may have unrealistic expectations, leading to feelings of disappointment post-surgery. |
| Necrosis of Tissue | Sometimes, insufficient blood supply can lead to tissue death, requiring further surgery. |
Risk Factors Influencing Complication Rates
Several factors can increase the likelihood of complications during or after panniculectomy:
- Pre-existing Conditions: Health issues such as diabetes, obesity, and autoimmune diseases can complicate recovery.
- Smoking: Nicotine hinders blood flow, significantly increasing the risk of wound healing issues and infections.
- Age: Older patients may experience longer recovery times and increased risks of cardiovascular complications.
- Medications: Certain medications, particularly those affecting blood clotting, may increase the risk of complications during surgery.
Mitigating Risks
While the potential risks and complications of panniculectomy surgery are significant, there are various strategies for mitigation. Effective pre-surgical consultations are paramount, ensuring that each patient is well-informed about the procedure and recovery expectations.
- Comprehensive Medical Evaluation: Prior to surgery, a thorough evaluation by the surgical team can identify any potential risks.
- Healthy Lifestyle Changes: Patients are encouraged to adopt a healthier lifestyle leading up to the surgery, which can include quitting smoking, achieving a healthy weight, and managing existing health conditions.
- Post-operative Care: Structured post-operative plans to monitor signs of infection and complications can help catch issues early.
Understanding the potential risks and complications associated with panniculectomy is essential in the decision-making process. Through careful consideration and planning with qualified healthcare professionals, patients can make informed choices that align with their health goals.
Benefits of Panniculectomy Surgery
Panniculectomy surgery offers numerous advantages for individuals burdened by excess abdominal skin. Often pursued following significant weight loss, this procedure not only enhances physical appearance but also delivers practical health benefits. Below is a detailed overview of the numerous advantages associated with this transformative procedure.
Physical Benefits
- Enhanced Contour: The most immediate benefit of panniculectomy surgery is the improvement in abdominal contour. By removing the excess skin, individuals often notice a flatter, tighter, and more aesthetically pleasing abdomen.
- Improved Mobility: Excess skin can hinder daily activities and physical movement. Post-surgery, many find increased comfort and flexibility during exercise and routine tasks. This newfound freedom can encourage a more active lifestyle, further promoting overall health.
- Clothing Fit: Many individuals report a significant improvement in how their clothes fit after the procedure. The elimination of excess skin allows for better fitting clothing, which can boost self-confidence and promote a more positive body image.
Health Benefits
- Reduced Skin Irritation: The presence of excess skin can lead to chafing and skin issues, such as rashes and infections. With the removal of the pannus (excess skin), many experience a substantial reduction in skin-related complaints.
- Improved Hygiene: The removal of excess skin folds allows for better hygiene. Patients can clean the abdominal area more effectively, potentially reducing the risk of infections that can occur in hidden skin folds.
- Relief from Physical Discomfort: Many individuals find that the weight of the excess skin causes discomfort, leading to back pain and other musculoskeletal issues. Panniculectomy alleviates this pressure, significantly enhancing overall physical well-being.
Psychological Benefits
- Increased Self-Esteem: The transformation that comes post-surgery can lead to notable improvements in self-esteem. Individuals often feel more comfortable in their own skin, which positively impacts their relationships and daily interactions.
- Motivation for Healthy Living: Successfully undergoing this surgery can serve as a motivational boost. Patients may feel inspired to maintain their weight loss and embrace healthier lifestyle choices, knowing they have taken a significant step toward improving their body.
- Psychological Well-Being: Beyond just self-esteem, many individuals report overall improvements in their mental health. The psychological lift from seeing the results can reduce anxiety and body image issues associated with significant weight loss.
Summary of Benefits
| Type of Benefit | Specific Advantages |
|---|---|
| Physical | Enhanced body contour, improved mobility, better fitting clothes. |
| Health | Reduced skin irritation, improved hygiene, relief from discomfort. |
| Psychological | Increased self-esteem, motivation for healthy living, better mental well-being. |
Panniculectomy surgery offers a holistic platform for transformative change in individuals facing the challenges of excess abdominal skin. With both tangible physical and psychological benefits, this procedure proves to be a more than just aesthetic decision; it often serves as a gateway to a healthier, more fulfilling lifestyle.
Cost Considerations for Panniculectomy
When contemplating the decision to undergo panniculectomy, financial factors play a significant role in the overall process. Understanding the costs involved can help individuals make informed choices. This section breaks down the various elements that contribute to the financial aspect of the surgery.
Initial Consultation Fees
Before scheduling the surgery, patients often meet with a board-certified plastic surgeon for an initial consultation. This meeting is crucial as it allows the surgeon to evaluate the individual’s specific case and discuss expectations. Typically, consultation fees range from $100 to $300. Some practices offer complimentary consultations, so it’s beneficial to research various clinics.
Surgical Costs
The costs associated with panniculectomy can vary widely based on a multitude of factors including:
- Geographic Location: Urban centers with a high demand for cosmetic procedures often charge more than rural areas.
- Surgeon’s Experience: Reputable and highly experienced surgeons may command higher fees, but they can yield better outcomes and reduced risks.
- Facility Fees: Costs will differ depending on whether the procedure takes place in a hospital or an outpatient surgical center.
Here’s a general breakdown of potential surgical costs:
| Cost Component | Estimated Range |
|---|---|
| Surgeon’s Fee | $3,000 – $10,000 |
| Anesthesia Fees | $600 – $1,200 |
| Facility Fees | $500 – $2,000 |
| Total Estimated Costs | $4,100 – $13,200 |
Additional Expenses
Beyond the direct costs of the surgery, patients should also consider several ancillary expenses, which may include:
- Pre-Surgical Testing: Blood tests, imaging, and other evaluations might range from $100 to $500.
- Post-Operative Care: Follow-up visits can accrue additional costs, often ranging from $100 to $300 per visit.
- Medications: Pain relief and antibiotics prescribed post-surgery can cost between $50 and $200.
Insurance Coverage
It’s important to note that insurance coverage for panniculectomy is complex. While some policies may cover the costs of surgery if deemed medically necessary (e.g., to address functional impairments caused by excess skin), others may classify it as a cosmetic procedure, thus leaving patients responsible for the full cost. Be sure to:
- Contact Insurance Provider: Verify coverage policies and necessary documentation to ensure eligibility.
- Obtain Medical Documentation: A letter from your healthcare provider explaining the medical necessity can be beneficial.
Financing Options
For individuals concerned about affordability, several financing options can ease the burden:
- Payment Plans: Many clinics offer payment plans, allowing patients to spread the cost over a set period.
- Medical Credit Cards: Companies like CareCredit allow patients to finance their medical expenses through specialized credit lines.
Summary
In summary, the cost considerations surrounding panniculectomy surgery encompass a wide range of aspects—from initial consultations and surgical fees to additional expenses and insurance coverage. Understanding these factors can greatly assist individuals in making informed decisions regarding their procedures. Exploring financing options and consulting with insurance providers can further mitigate potential financial stress, making this transformative surgery more accessible. Always ensure that you perform thorough research and seek multiple quotes to refine your understanding of the financial implications involved in panniculectomy.
FAQs about Panniculectomy Surgery
Engaging in a major surgical procedure like panniculectomy can inevitably lead to a myriad of questions. Understanding this surgery’s dynamics—ranging from the procedure itself to post-operative care—can alleviate anxieties and prepare potential candidates for what lies ahead. Here are some frequently asked questions to provide clarity and information about panniculectomy.
| Question | Answer |
|---|---|
| What is the difference between panniculectomy and tummy tuck? | While both procedures involve the removal of excess skin, a tummy tuck is often performed for cosmetic enhancement, focusing on tightening the abdominal wall, whereas panniculectomy is primarily for medical necessity, focusing on health improvement and stability with minimal cosmetic objectives. |
| How long does the surgery take? | Typically, the duration of the surgery ranges from 2 to 5 hours, depending on the extent of the skin removal required and the specific conditions of the patient involved. |
| Is panniculectomy covered by insurance? | In many cases, health insurance may cover this procedure if it is deemed medically necessary, such as when excess skin causes physical discomfort or contributes to health issues such as skin infections. It’s recommended to consult your insurance policy beforehand. |
| What type of anesthesia is used during the procedure? | Most panniculectomies are performed under general anesthesia, ensuring the patient is completely asleep during the operation. In some cases, a local anesthetic may be utilized for targeted areas, depending on the patient’s specific needs and the surgeon’s recommendations. |
| How long is the recovery period? | Recovery times can vary, but generally, initial healing can take from 2 to 6 weeks, while complete recovery may extend up to several months. The recovery timeline largely depends on individual health, the extent of the surgery, and adherence to post-operative care instructions. |
| Will there be visible scars after surgery? | Yes, scarring is an inevitable aspect of the procedure. However, skilled surgeons aim to minimize and strategically place incisions to ensure that scars are as discreet as possible. These tend to fade over time, becoming less noticeable with appropriate post-operative care. |
| Can I return to work immediately after the surgery? | It is advisable to take time off work, typically ranging from 2 to 6 weeks, depending on the job’s physical demands and the individual’s healing process. Discussing this aspect with your healthcare provider can help outline a tailored recovery timeline. |
| What activities should be avoided after surgery? | Patients should refrain from heavy lifting, strenuous exercise, and any activity that places strain on the abdominal area during the early recovery phase. Gradually reintroducing activities in consultation with a healthcare provider is crucial for optimal recovery. |
| Are there any long-term effects from the surgery? | Long-term effects can vary; most individuals report substantial improvements in mobility, comfort, and self-esteem. However, some patients might experience residual swelling or changes in skin sensation. Regular follow-ups with healthcare providers can help monitor recovery and address any concerns. |
Navigating through the intricacies of panniculectomy helps to empower individuals considering the procedure. Having an established understanding of common inquiries regarding this surgery can enhance the decision-making process and potentially lead to a more positive outcome. Engaging with medical professionals and surgical teams before and after the operation will also ensure a thorough understanding of the expectations surrounding this transformative journey.
Frequently Asked Questions
What is a panniculectomy surgery?
Panniculectomy surgery is a surgical procedure that involves the removal of excess skin and fat tissue from the lower abdomen, primarily to improve comfort, hygiene, and aesthetic appearance. This condition, often caused by significant weight loss or pregnancy, results in a sagging fold of skin known as a pannus. The surgery focuses on excising this excess tissue without major alteration to the abdominal muscles, distinguishing it from a complete tummy tuck.
Who is a suitable candidate for panniculectomy?
Individuals who have undergone significant weight loss — whether through diet, exercise, or bariatric surgery — are often ideal candidates for panniculectomy. Furthermore, those experiencing physical discomfort, rashes, or hygiene issues due to excess abdominal skin may also qualify for the procedure. Typically, candidates should be in good overall health, maintain a stable weight, and have realistic expectations regarding the surgery’s outcomes.
What is the recovery process like after panniculectomy surgery?
The recovery process after a panniculectomy surgery typically involves an initial period of discomfort, swelling, and bruising. Patients are advised to take time off work, usually around 2-4 weeks, depending on the nature of their job. Activity restrictions may include avoiding heavy lifting and strenuous exercise for several weeks. Follow-up appointments are essential to monitor healing and to remove sutures or drains, if necessary. Complete healing can take several months, and the final results will gradually become more apparent as swelling subsides.
What are the potential risks and complications associated with panniculectomy?
As with any surgical procedure, panniculectomy carries potential risks, including infection, bleeding, scarring, and complications related to anesthesia. Additionally, some patients may experience delayed healing or dissatisfaction with aesthetic results. It is crucial to consult with a qualified surgeon to understand and weigh these risks against the expected benefits to ensure an informed decision before proceeding with the surgery.
Will I have visible scarring after panniculectomy surgery?
Yes, like most surgical procedures that involve incisions, panniculectomy surgery will typically result in some visible scarring. The extent and location of the scars can vary considerably based on individual healing processes, the technique used by the surgeon, and post-operative care. Patients are encouraged to follow their surgeon’s pre- and post-surgery care instructions, as well as to discuss options for minimizing scarring, such as silicone sheeting or scar creams, during their consultation.