Retroperitoneal lymph node dissection, commonly referred to as RPLND surgery, plays a crucial role in the treatment of certain cancers, particularly testicular cancer. As an intricate procedure aimed at removing lymph nodes located in the retroperitoneal space, understanding its purpose and implications is essential for anyone facing this surgery. Throughout this comprehensive guide, we will delve into the various aspects of RPLND, from the indications that warrant this procedure to the detailed steps involved during the surgery itself. Furthermore, we will address the recovery process, potential risks, and strategies for managing discomfort, ensuring that patients feel informed and supported every step of the way. Whether you are preparing for surgery or seeking to understand the procedure for a loved one, this guide aims to provide valuable insights and essential information to empower you in your journey.
Understanding RPLND Surgery: An Overview
Retroperitoneal lymph node dissection, commonly referred to as RPLND, is a surgical procedure primarily aimed at the evaluation and management of cancers, particularly testicular cancer. This surgery involves the removal of lymph nodes located in the retroperitoneal space, which is situated at the back of the abdominal cavity. The primary goal of RPLND is not only to assess the presence of cancer but also to potentially eradicate cancerous tissues that may spread to lymph nodes, thereby improving overall patient prognosis.
Importance of RPLND Surgery
RPLND is a critical component of cancer treatment strategies for individuals diagnosed with specific types of tumors, especially germ cell tumors. Understanding its role in the surgical management of cancer can be broken down into key benefits:
| Key Benefits of RPLND Surgery | Description |
|---|---|
| Accurate Staging | RPLND helps determine the extent of cancer spread, guiding treatment decisions. |
| Potential for Cure | By removing affected lymph nodes, surgery may eliminate the cancer entirely, reducing recurrence risks. |
| Promotes Survival Rates | Studies indicate that timely intervention through RPLND can significantly enhance survival probabilities for testicular cancer patients. |
| Supportive for Chemotherapy | For some patients, RPLND can help enhance the effectiveness of subsequent chemotherapy by removing residual cancerous tissues. |
Who is a Candidate for RPLND?
The candidacy for RPLND varies according to multiple factors, including but not limited to the patient’s overall health, the specific type and stage of cancer, and previous treatments. Typically, individuals with the following conditions may be considered:
- Stage I Testicular Cancer: Patients diagnosed with stage I testicular cancer, where cancer cells have not spread beyond the testes.
- Residual Disease Post-Chemotherapy: Patients who have undergone chemotherapy and still show signs of residual disease may be evaluated for RPLND.
- High-Grade Non-Seminomatous Germ Cell Tumors: Those with aggressive tumor types may require this surgical procedure to manage their cancer effectively.
The Role of RPLND in Cancer Management
RPLND plays a vital role in the comprehensive management of testicular cancer and related conditions. The procedure enhances the knowledge around a patient’s cancer level and specifically targets those areas likely to harbor undetected metastases, fundamentally altering treatment trajectories. Besides addressing cancer directly, RPLND serves diagnostic purposes, allowing for thorough pathological assessments of lymph nodes that inform future treatment strategies.
The Impact of RPLND on Quality of Life
While RPLND is guided by medical indications, it also significantly affects the patient’s quality of life. After the procedure, many individuals report improvements in both physical and emotional well-being due to reduced cancer burden. Nonetheless, it is crucial for patients and their families to remain informed about the potential challenges that may arise during recovery.
In sum, RPLND surgery represents an essential intervention in the landscape of cancer treatment, particularly for testicular cancers. Understanding its purpose, benefits, and applicability is integral for patients embarking on this medical journey. Such awareness empowers individuals to make informed decisions alongside their healthcare teams, enhancing treatment outcomes and fostering clearer expectations for their overall care.
Indications for Retroperitoneal Lymph Node Dissection
Retroperitoneal lymph node dissection (RPLND) is a specialized surgical procedure primarily employed to address issues related to certain types of cancers, particularly testicular cancer. Recognizing the indications for RPLND is crucial for both patients and healthcare professionals, as it helps to ensure that the procedure is performed when it is most beneficial. Below are some key indications for RPLND, presented in a clear and organized table for ease of understanding.
| Indication | Description |
|---|---|
| Testicular Cancer | RPLND is frequently indicated for patients with non-seminomatous testicular germ cell tumors, specifically when there is evidence of lymph node involvement. |
| Residual Lymphadenopathy | If imaging tests (such as CT scans) reveal persistent enlarged lymph nodes following treatment for testicular cancer, RPLND may be necessary to remove these residual masses. |
| Staging and Evaluation | In cases where essential information regarding tumor staging cannot be obtained through non-invasive means, RPLND can provide vital insights into the extent of cancer spread. |
| Treatment of Lymphatic Recurrence | RPLND is indicated for those who have experienced a recurrence of cancer within the lymphatic system after previous treatment, as it serves to eliminate the affected nodes. |
| Tumor Marker Elevation | Elevated tumor markers (like alpha-fetoprotein or human chorionic gonadotropin) after treatment may indicate potential residual disease requiring surgical intervention. |
Understanding the Context of Indications
The primary indication for RPLND relates directly to managing testicular cancer. Testicular cancer often metastasizes to retroperitoneal lymph nodes, making it imperative that any affected nodes be assessed and, if necessary, removed. The success rate of RPLND in treating this condition significantly increases when lymph node involvement is identified early.
Additional Considerations
- Patient Symptoms: Patients presenting symptoms such as abdominal pain, unexplained weight loss, or swollen lymph nodes may warrant further examination, which could lead to RPLND if cancer involvement is suspected.
- Adjuvant Treatment: RPLND might also serve as a follow-up procedure after chemotherapy or radiation therapy, primarily in cases where complete tumor regression is questionable based on follow-up imaging.
- Multi-disciplined Approach: RPLND is often performed in conjunction with consultations from oncologists, urologists, and radiologists, ensuring a comprehensive approach to treatment that addresses all aspects of cancer care.
- Long-term Monitoring: Candidates for RPLND should be informed about the necessity of ongoing monitoring and evaluation after the procedure to ensure the effectiveness of the surgery and assess for any possible recurrence.
By comprehensively understanding the indications for RPLND, patients and their families can engage in informed discussions with their healthcare providers about the necessity and potential benefits of this significant surgical intervention.
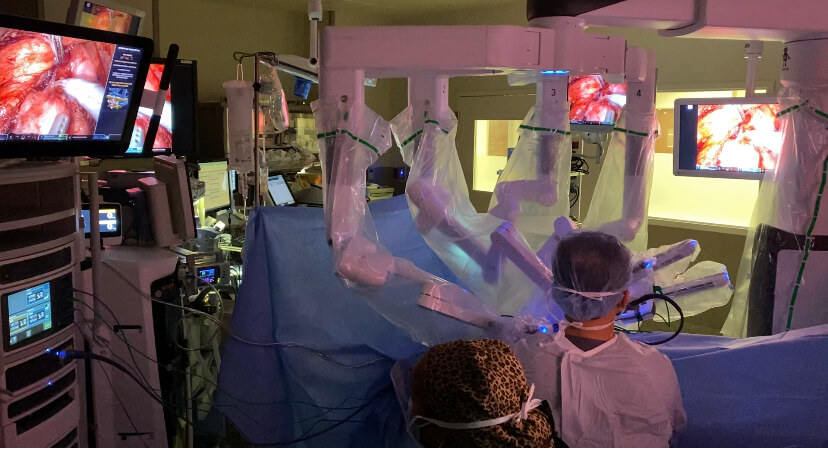
The Surgical Procedure: Step-by-Step
Retroperitoneal lymph node dissection (RPLND) is a complex surgical procedure often utilized to treat certain types of cancer, particularly testicular cancer. Understanding the steps involved in this surgery can help demystify the process for patients and their families. This detailed overview outlines the sequence of events from the initial preparation through to the completion of the surgery.
Preoperative Steps
Prior to the surgical procedure, several preparatory measures are taken:
| Step | Description |
|---|---|
| Medical Evaluation | A thorough assessment that includes physical examinations, imaging studies, and possibly lab tests. |
| Informed Consent | Patients are educated about the procedure, risks, and alternatives, signing consent forms to proceed. |
| Anesthesia Consultation | A meeting with the anesthesiologist to discuss types of anesthesia and any relevant medical history. |
Anesthesia Administration
Once the patient is in the operating room, the next step involves anesthesia administration. RPLND typically requires general anesthesia, meaning the patient will be completely asleep and unaware during the procedure. The anesthesiologist carefully monitors the patient’s vital signs throughout the surgery.
Surgical Exposure
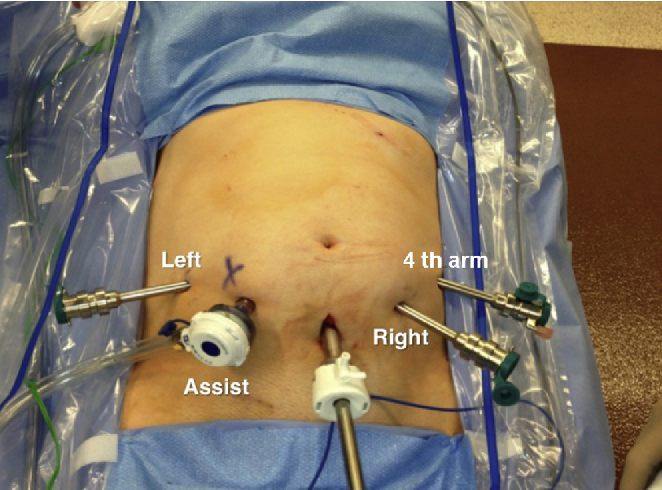
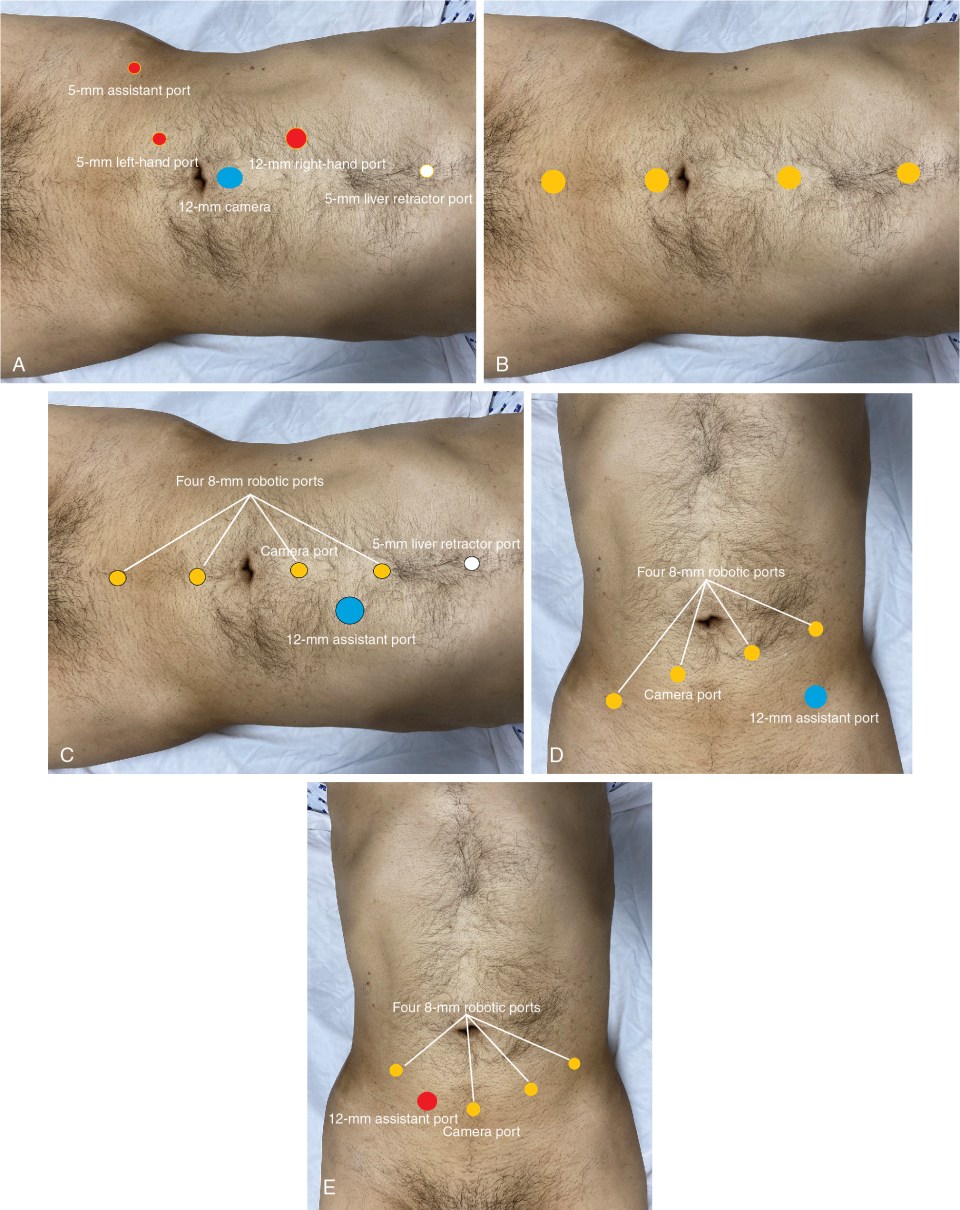
The actual dissection can vary depending on the individual case, but the following general steps are commonly employed:
- Incision: A midline abdominal incision is frequently made to provide access to the retroperitoneal space. In some cases, a bilateral or flank approach may be used.
- Exploration: The surgeon inspects the abdominal cavity and identifies the surrounding structures, ensuring there are no pre-existing complications.
Dissection of Lymph Nodes
The core objective of RPLND is the dissection of the lymph nodes. The steps involved here include:
- Identification: The targeted lymph nodes, commonly found around the aorta and inferior vena cava, are located.
- Separation: Surrounding tissues are carefully dissected away to preserve adjacent structures, including blood vessels and nerves.
- Removal: Once adequately exposed, the affected lymph nodes are removed. This may also include nearby tissue, if deemed necessary, based on the extent of the cancer.
Hemostasis and Closure
Following the lymph node extraction, it’s crucial to control any bleeding:
- Hemostasis: The surgeon uses various techniques to ensure that bleeding vessels are secured, minimizing the risk of postoperative complications.
- Drainage Placement: In some cases, a drain may be placed to prevent fluid accumulation, which is common after such extensive procedures.
- Closure: The surgeon carefully closes the incision using sutures or staples, considering aesthetic factors as well as healing.
Postoperative Transition
After the surgery, the patient is moved to the recovery area for monitoring as the effects of anesthesia wear off. Healthcare professionals assess the patient’s vital signs, manage pain, and ensure the patient remains stable before progressing to more extensive recovery.
This step-by-step breakdown not only clarifies the technical aspects of RPLND but also highlights the meticulous nature of the procedure. Understanding each stage can alleviate fears and anxiety surrounding the surgery, providing patients and their families with a clearer perspective on what to expect during this critical treatment.
Recovery Process After RPLND Surgery
Recovering after retroperitoneal lymph node dissection (RPLND) is a multifaceted journey that requires careful attention and a proactive approach. The recovery phase is critical for the overall success of the surgery and for the restoration of normal bodily functions. On average, patients can expect varying timelines for recovery, but understanding the process can significantly ease anxiety and promote a smoother return to everyday life.
Immediate Post-Surgery Care
After the surgical procedure, patients typically spend a few hours in a recovery room under constant monitoring. Initially, medical staff will observe vital signs such as heart rate, breathing, and blood pressure. During this time, pain management is a priority, as anesthesia and the nature of the procedure can lead to significant discomfort.
Key Aspects of Immediate Post-Surgery Care:
| Aspect | Description |
|---|---|
| Vital Monitoring | Continuous observation of heart rate, breathing, and blood pressure. |
| Pain Management | Administration of analgesics and pain-relief protocols as needed. |
| Fluid & Nutrition | Intravenous fluids are given until oral intake is allowed. |
| Mobility Support | Assistance for short walks to encourage movement and prevent complications. |
Hospital Stay
The length of stay in the hospital following the procedure typically ranges from two to five days, depending on individual recovery progress and complications, if any. During this time, healthcare providers will continue to focus on pain management and start mobilizing patients to minimize the risk of blood clots and further complications.
Return to Daily Activities
Returning to normal activities is a gradual process, and it’s crucial to heed the advice of healthcare providers. Here’s a general guideline for returning to daily routines:
| Activity | Timeline |
|---|---|
| Light Activities | Within 1-2 weeks post-surgery, such as light walking. |
| Moderate Activities | 2-4 weeks after the procedure, such as household chores. |
| Strenuous Activities | Generally, after 6-8 weeks, including heavy lifting or vigorous exercise. |
Pain and Discomfort Management
Discomfort following RPLND can be effectively managed through a combination of prescribed medications and home care strategies. Patients may experience soreness around the incision site, abdominal cramps, or fatigue. It’s crucial to report any abnormal pain or symptoms to a healthcare provider immediately.
Strategies for Pain Management:
| Strategy | Details |
|---|---|
| Medications | Follow prescribed pain relief regimen. |
| Ice Therapy | Application of ice packs to reduce swelling and soreness. |
| Rest | Prioritize sleep and relaxation. |
| Gentle Movement | Engage in light stretching and walking as recommended. |
Follow-Up Appointments
Routine follow-up appointments are essential in monitoring recovery and detecting any potential complications early. Regular visits will also help in assessing cancer recurrence in the case of malignancies. These appointments enable healthcare professionals to adjust any treatment plans based on the patient’s progress.
By prioritizing recovery efforts and being mindful of the body’s healing cues, individuals can significantly enhance their recovery journey post-RPLND surgery. Emphasizing support from healthcare teams and loved ones can provide emotional comfort and improve resilience during this challenging phase.
Managing Pain and Discomfort Post-Surgery
Experiencing pain and discomfort after undergoing retroperitoneal lymph node dissection is a common occurrence. The body goes through significant changes as it heals from such a comprehensive surgical procedure. However, proper management techniques can greatly aid patients in navigating this healing phase with more comfort. This section delves into the various strategies for managing pain and discomfort following this intricate surgery.
Pain Management Strategies
An effective pain management plan includes both pharmacological and non-pharmacological methods. Here’s a detailed overview:
| Method | Description |
|---|---|
| Medications | Opioid pain relievers may be prescribed for moderate to severe pain during the initial days of recovery. Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help reduce pain and inflammation. Always follow your physician’s instructions regarding dosages. |
| Local Anesthetics | In some cases, healthcare providers may administer local anesthetics to numb the surgical site, providing immediate relief. Options can include nerve blocks, which can reduce pain sensations effectively. |
| Physical Therapy | Engaging in light physical therapy can enhance blood flow and promote a quicker recovery. Gentle exercises guided by a therapist can also help alleviate pain and stiffness. |
| Heat and Cold Therapy | Applying ice packs can help minimize swelling and numb the area, while heat therapy, such as a warm compress, can soothe muscle tension and promote relaxation. Alternate between heat and cold as needed. |
| Relaxation Techniques | Techniques such as deep breathing exercises, meditation, and controlled visualization can contribute significantly to pain reduction by promoting relaxation and reducing stress. |
| Supportive Care | Family and friends can play a critical role in providing emotional support, which can indirectly reduce the perception of pain. Simple comforts such as a warm blanket or a favorite movie can make a big difference. |
Recognizing and Communicating Pain Levels
Each individual experiences pain differently, which makes it crucial to recognize and communicate pain levels effectively. Using a pain scale ranging from 0 (no pain) to 10 (worst possible pain) can help patients convey their pain experiences clearly to healthcare providers. This communication allows medical professionals to adjust pain management strategies accordingly.
Signs of Abnormal Discomfort
While some pain and discomfort are expected after surgery, certain signs require immediate medical attention. Patients should watch for:
- Excessive Swelling or Redness: Development of increased swelling or redness around the incision sites may indicate infection or other complications.
- Fever: A persistent or rising fever may signal infection and should be reported to a healthcare provider.
- Severe or Uncontrolled Pain: Pain that does not improve with medication or worsens over time should be addressed by your doctor.
Evaluating Pain Management Effectiveness
To ensure that pain and discomfort are being effectively managed, patients should regularly evaluate their pain relief strategies. Patients can create a simple daily log documenting:
- Pain intensity at various intervals
- Times when medications were taken
- Activities that aggravated or alleviated pain
Seeking Support
Finally, engaging in support groups or talking with a mental health professional can provide additional avenues for emotional support. These discussions can help address both the physical and emotional aspects of recovery, ultimately leading to a more holistic healing process.
By combining these strategies, patients can effectively manage pain and discomfort while focusing on recovery after undergoing retroperitoneal lymph node dissection. It’s essential to take an active role in pain management for the most beneficial healing journey.
Expected Outcomes and Success Rates
When considering retroperitoneal lymph node dissection surgery, a crucial aspect for patients is understanding the expected outcomes and success rates associated with the procedure. This surgery is often performed to treat certain types of cancer, particularly testicular cancer, as it aids in the removal of potentially malignant lymph nodes that could harbor cancerous cells. Here, we will explore the various outcomes patients can anticipate following the procedure and examine the statistical success rates linked to it.
Key Expected Outcomes
The success of retroperitoneal lymph node dissection surgery can be assessed through several pivotal outcomes:
| Outcome | Description |
|---|---|
| Tumor Clearance | The primary goal of this surgery is to achieve complete removal of cancerous lymph nodes. In many cases, surgeons successfully excise tumor-involved nodes, which can significantly reduce the risk of cancer recurrence. |
| Reduction in Tumor Markers | A measurable decrease in tumor markers post-surgery often indicates effective removal of cancerous tissue. In cases of testicular cancer, for instance, levels of alpha-fetoprotein (AFP) and human chorionic gonadotropin (hCG) may drop significantly. |
| Improved Prognosis | Patients who undergo the surgery may experience a better prognosis, especially when the surgery is performed in early-stage testicular cancer. This can lead to increased overall survival rates, as discussed further below. |
| Quality of Life Improvements | Many patients report enhanced quality of life post-surgery, especially if the procedure successfully eliminates cancerous threats and alleviates associated symptoms. |
Success Rates
The success rates of retroperitoneal lymph node dissection surgery can vary based on several factors, including the individual’s overall health, cancer type, and cancer stage at diagnosis. However, research indicates promising statistics:
| Cancer Type | Success Rate |
|---|---|
| Early-stage Testicular Cancer | 90-95% |
| Non-seminomatous germ cell tumors | 70-80% |
| Relapsed Testicular Cancer | 50-60% |
These percentages reflect the likelihood of achieving tumor-free status following the procedure. When the cancer is detected early and is not extensively spread, the success rate is generally higher.
Long-term Outcomes
In addition to immediate success rates, long-term outcomes are significant indicators of the surgery’s effectiveness. Patients who undergo successful lymph node dissection may experience:
- Lower Recurrence Rates: The surgery significantly minimizes the chance for recurrence, especially in early-stage cancers. Studies indicate that, with effective treatment, recurrence rates can be as low as 5-10% for early-stage testicular cancer.
- Long-Term Survival Statistics: Many researchers suggest that patients with non-seminomatous germ cell tumors have an overall survival rate exceeding 85% over a five-year period when treated appropriately.
Conclusion
Understanding the expected outcomes and success rates of retroperitoneal lymph node dissection surgery can empower patients to make informed decisions regarding their treatment options. Focusing on early detection and intervention tends to yield the best prognosis and overall quality of life after surgery. Through comprehensive follow-up care and vigilant monitoring, patients can continue to enhance their health post-operation and maintain a positive outlook on their prognosis.
Emotional and Psychological Support for Patients
Undergoing a significant surgical procedure, such as retroperitoneal lymph node dissection, can present a range of emotional and psychological challenges for patients. As the body copes with the physical trauma of surgery, it is equally important to address the emotional turmoil that may arise. The journey toward recovery is not only about physical healing but also the mental and emotional well-being of the patient.
Understanding Emotional Responses
Many individuals undergoing this type of surgery experience a variety of emotions, including anxiety, fear, uncertainty, and sometimes depression. These feelings are completely normal and can stem from concerns about the surgery itself, potential outcomes, and the subsequent recovery journey. Recognizing that these emotional responses are common is essential for patients and their loved ones.
Common Emotional Responses
| Emotion | Description |
|---|---|
| Anxiety | Worrying about surgery, potential complications, and future health outcomes. |
| Fear | Fears related to the procedure, hospital environment, and body changes. |
| Uncertainty | Concerns about what life will look like post-surgery, both physically and mentally. |
| Depression | Feelings of sadness or hopelessness that can impact motivation and daily activities. |
The Importance of Support Systems
Building a robust support system is fundamental for navigating the challenges that arise before, during, and after surgery. Loved ones, including family members and friends, can provide emotional stability and encouragement. They can share their thoughts and feelings, lending an open ear or a reassuring presence, which can significantly alleviate anxiety.
Professional Support Options
While personal support from loved ones is invaluable, seeking professional psychological support is equally important. Mental health professionals, such as therapists or counselors, can help patients process their emotions in a healthy manner. Here are some forms of professional support available:
| Support Type | Description |
|---|---|
| Individual Therapy | One-on-one sessions focusing on personal emotions and coping strategies. |
| Support Groups | Group sessions (in-person or virtual) to connect with others undergoing similar experiences. |
| Cognitive Behavioral Therapy (CBT) | A structured approach to help patients manage their emotions and thoughts. |
Mindfulness and Stress Relief Techniques
In addition to external support systems, patients can engage in self-care practices that promote emotional well-being. Techniques such as mindfulness, meditation, deep breathing exercises, and gentle physical activity (like yoga or walking) can help reduce anxiety and improve mood. These practices encourage patients to stay grounded, enhance their mental clarity, and foster a sense of control over their recovery.
Open Communication
Patients should not hesitate to communicate their feelings and concerns with healthcare providers. Open dialogues about emotional and psychological health allow for tailored support structures to be established. Healthcare professionals can suggest additional resources, including support groups or mental health referrals, ensuring that every aspect of the patient’s health is prioritized.
The Role of Family and Friends
Family and friends play a critical role in a patient’s emotional recovery. Encouraging loved ones to engage actively in the recovery process, whether by attending appointments or participating in daily activities, helps to reinforce feelings of belonging and support. It provides patients with a network of empathy and understanding, which is vital for emotional healing.
Affording attention to emotional and psychological aspects during the recovery from retroperitoneal lymph node dissection can make a significant difference in the overall recovery experience. By recognizing the emotional challenges, leveraging support systems, and practicing self-care, patients can navigate the complex landscape of their recovery journey more effectively.
Follow-Up Care and Monitoring After RPLND
After undergoing retroperitoneal lymph node dissection, diligent follow-up care and monitoring play a crucial role in a patient’s overall recovery and long-term health. These measures not only help address any potential complications but also ensure that patients benefit from optimal health management following their surgery. Below is a detailed breakdown of what patients can expect during their follow-up care journey.
Importance of Follow-Up Visits
Regular follow-up visits enable healthcare providers to monitor the patient’s recovery progress and detect any complications early. Typically, these are scheduled weekly or biweekly right after surgery, transitioning to monthly or quarterly visits as recovery progresses. The frequency of these appointments may vary based on individual recovery rates and specific clinical situations.
Key Components of Follow-Up Care
The follow-up care typically involves the following components:
| Component | Description |
|---|---|
| Physical Examinations | Upon each visit, healthcare professionals perform a comprehensive physical examination, focusing on the surgical site and assessing overall health. |
| Imaging Studies | Imaging techniques like CT scans, MRI, or ultrasounds may be employed to monitor the lymph nodes and surrounding tissues for any abnormalities or recurrence. |
| Blood Tests | Blood work is essential in these follow-ups. Tests might include tumor marker levels and routine blood counts to assess organ function and overall health. |
| Symptom Assessment | Patients are asked about any new symptoms, pain levels, or discomfort. This feedback assists doctors in tailoring individual care strategies. |
| Education and Support | Healthcare providers offer valuable information on lifestyle changes, dietary habits, and managing the emotional effects of surgery, ensuring holistic patient care. |
Managing Complications
During follow-up visits, it is critical to monitor for possible complications such as infection, lymphatic fluid buildup, and pain management issues. Early detection can lead to prompt treatment, significantly reducing the risk of long-term health implications.
Psychological Support
The aftermath of significant surgeries, such as RPLND, can yield substantial emotional and psychological challenges. During follow-up appointments, healthcare providers will not only address physical recovery but also the mental and emotional state of the patient. Support groups, counseling, or recommendations for mental health professionals may be offered to aid in coping with anxiety or depression.
Long-Term Monitoring
Depending on the initial findings post-surgery and patient health status, continuous long-term surveillance may be necessary. Patients usually require periodic imaging and blood tests for several years following surgery to ensure the absence of cancer recurrence. This ongoing monitoring is not just limited to a specific timeframe; research suggests that a substantial follow-up phase can extend up to 10 years for certain patients.
Tips for Patients
To maximize the benefits of follow-up care, patients should consider these practical tips:
- Keep a symptom diary to note changes and concerns that arise between appointments.
- Maintain open communication with all healthcare providers regarding any new medications or treatments.
- Follow the recommended lifestyle modifications, including diet and exercise, as these positively impact recovery.
In summary, diligent follow-up care and monitoring after retroperitoneal lymph node dissection significantly contribute to a patient’s recovery experience. Engaging with healthcare professionals and adhering to the recommended follow-up schedule is essential for maintaining health and addressing potential complications effectively.
Frequently Asked Questions
What is RPLND surgery and why is it performed?
Retroperitoneal Lymph Node Dissection (RPLND) is a surgical procedure primarily used in the treatment of testicular cancer. It involves the removal of lymph nodes located in the retroperitoneal space, which is situated behind the abdominal cavity. RPLND is performed to diagnose and treat cancer that may have spread to these lymph nodes, to determine the presence of cancer recurrence, and to achieve better long-term outcomes for patients. By removing affected lymph nodes, surgeons aim to reduce the risk of metastasis and increase the chance of successful treatment.
What can patients expect during the recovery process after RPLND surgery?
Recovery after RPLND surgery varies from person to person but generally entails a hospital stay of several days. Patients can expect some post-operative discomfort, which may include pain or swelling in the abdomen. It is crucial to follow the doctor’s postoperative care plan, which typically includes prescribed pain management, activity restrictions, and follow-up appointments for monitoring recovery. Most patients can gradually resume normal activities within six to twelve weeks, although full recovery may take longer. It’s essential to prioritize rest and communicate any concerning symptoms to healthcare providers.
What are the potential risks and complications associated with RPLND surgery?
Like any surgical procedure, RPLND surgery carries potential risks and complications. Common risks include infection, bleeding, injury to surrounding organs or nerves, and lymphatic fluid accumulation. A significant complication can be the development of complications related to the surgical site, which may lead to prolonged recovery. Additionally, some patients might experience changes in fertility or hormonal function after the procedure. Proper preoperative evaluation and skilled surgical technique are crucial in minimizing these risks.
How does RPLND surgery impact future fertility options for male patients?
RPLND surgery can have implications on male fertility, as it involves the removal of lymph nodes near the reproductive organs. In some cases, this procedure may affect semen quality or hormone levels. Patients concerned about their fertility before the surgery are encouraged to discuss sperm banking options with their healthcare provider. Advances in surgical techniques, including nerve-sparing methods, are being employed to mitigate fertility risks, but patients should always have an in-depth conversation about potential outcomes with their oncologist.
What is the role of RPLND in the treatment of non-seminomatous testicular cancer?
RPLND plays a critical role in the management of non-seminomatous testicular cancer, which is known for its tendency to spread to retroperitoneal lymph nodes. This surgical procedure is typically recommended after chemotherapy when imaging studies indicate residual masses in the lymph nodes. RPLND helps assess whether cancer is still present and allows for the removal of any remaining cancerous tissue, which can lead to better prognosis and reduced recurrence rates. In some scenarios, RPLND might be performed as the initial treatment if the disease is detected at early stages.