Embarking on the journey to regain mobility and alleviate pain can be daunting, especially when considering a significant medical procedure like the total knee replacement procedure. If you are among the millions of adults facing debilitating knee issues due to arthritis or injury, understanding what lies ahead can empower you to make informed decisions. In this comprehensive guide, we will walk you through every aspect of the process—from the initial assessment to post-operative care and rehabilitation. By the end of this post, you will have a clear blueprint of what to expect, enabling you to approach your surgery with confidence and ease.
What is Total Knee Replacement?
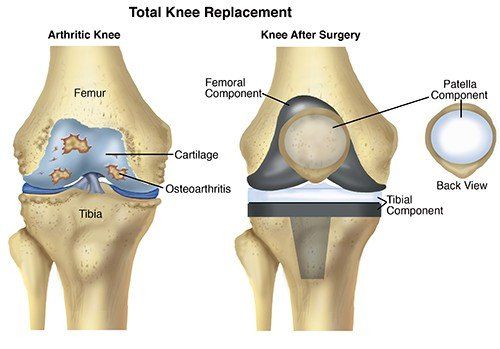
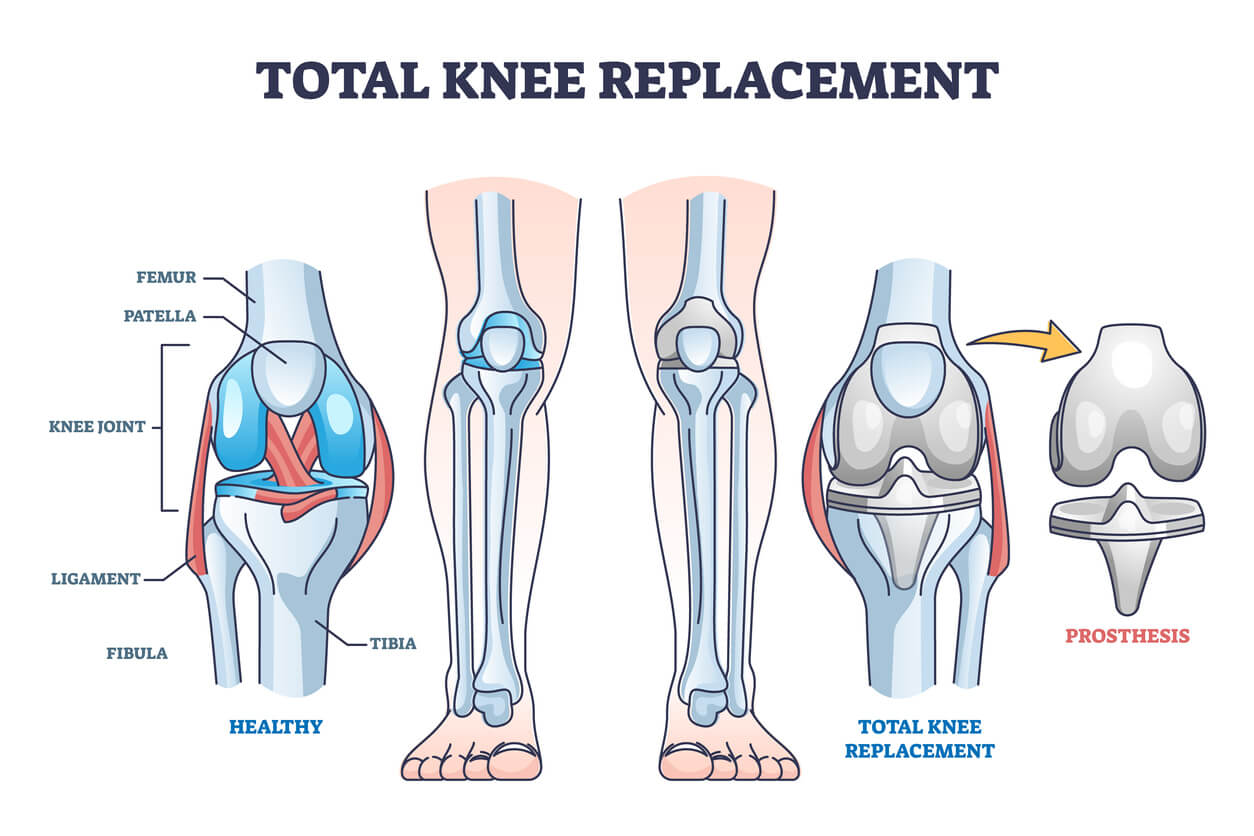
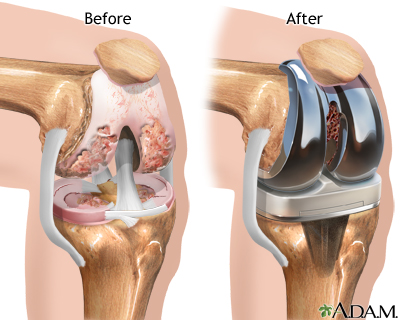
Total knee replacement (TKR) is a surgical procedure designed to relieve pain and restore function in patients suffering from severe knee damage, typically caused by osteoarthritis, rheumatoid arthritis, or post-traumatic arthritis. During the procedure, surgeons replace damaged or worn-out cartilage and bone with artificial components, primarily made from metal and plastic. This operation is considered one of the most successful interventions in orthopedic surgery, effectively alleviating knee pain and improving quality of life for millions of individuals worldwide.
Anatomy of the Knee
To better understand the total knee replacement procedure, it’s essential to comprehend the anatomy of the knee joint, made up of three bones:
| Bone | Description |
|---|---|
| Femur | The thigh bone, which connects to the knee joint. |
| Tibia | The shin bone, forming the lower leg’s base. |
| Patella | The kneecap, resting in front of the joint to provide protection. |
In a healthy knee, the ends of these bones are covered with a smooth cartilage, allowing for fluid movement. However, with the excessive wear and tear or inflammation, this cartilage can deteriorate, leading to bone-on-bone contact, resulting in stiffness, swelling, and pain.
Goals of Total Knee Replacement
The primary goals of total knee replacement include:
- Pain Relief: Significantly reducing or completely alleviating throughout knee discomfort.
- Improved Functionality: Enhancing mobility, stability, and range of motion in the knee joint.
- Reduced Stiffness: Gaining greater flexibility to facilitate daily activities and improve overall quality of life.
Indications for Total Knee Replacement
Total knee replacement surgery is recommended under specific conditions that indicate severe degeneration of the knee joint. The following factors typically warrant consideration for TKR:
- Persistent knee pain that limits daily activities or leads to a decreased quality of life.
- Inadequate response to conservative treatments such as medications, physical therapy, or injections.
- Joint stiffness severely restricting movement, affecting fundamental tasks like walking or climbing stairs.
- Deformities of the knee, such as bowing or knock-knees, resulting from arthritis progression.
Types of Total Knee Replacement
There are two primary types of TKR procedures:
- Total Knee Replacement: Involves replacing both the femoral and tibial surfaces as well as the patella.
- Partial Knee Replacement: Involves resurfacing only one compartment of the knee, preserving healthy bone and cartilage in other sections.
Total knee replacements utilize advanced surgical techniques that leverage technology such as computer navigation and robotic assistance, allowing for more precise alignment and reduced complications.
Summary
In essence, a total knee replacement procedure serves as a pivotal solution for individuals suffering from debilitating knee conditions. By replacing the damaged joint surfaces with artificial components, the surgery not only helps alleviate pain but significantly enhances mobility, enabling patients to engage in everyday activities with ease and enjoyment. If you are considering this procedure, it’s vital to consult with an orthopedic specialist to evaluate your specific situation and determine the most appropriate course of action.
Indications for Total Knee Replacement
The total knee replacement procedure is a significant surgical intervention, typically recommended for patients experiencing chronic knee pain and functional limitations due to various underlying conditions. Understanding the indications for this procedure is essential for patients as they contemplate their options. Below are the primary factors that may lead an orthopedic surgeon to recommend a total knee replacement.
Common Indications
| Indication | Description |
|---|---|
| Osteoarthritis | The most prevalent reason for knee replacement, osteoarthritis involves the degeneration of cartilage, leading to pain, stiffness, and loss of mobility. Patients often experience increased symptoms during weight-bearing activities. |
| Rheumatoid Arthritis | An autoimmune disorder, rheumatoid arthritis can cause inflammation and damage to the knee joints, resulting in significant pain and diminished function. This condition often necessitates surgical intervention when non-surgical treatments fail to relieve symptoms. |
| Post-Traumatic Arthritis | Injury to the knee, such as fractures or ligament tears, can lead to post-traumatic arthritis. Over time, deteriorating joint function and chronic pain may develop, prompting consideration of a total knee replacement. |
| Avascular Necrosis | This condition occurs when the blood supply to the bone is disrupted, resulting in bone tissue death. Avascular necrosis can lead to severe joint pain and limited mobility, often necessitating surgical intervention when conservative options are exhausted. |
| Failed Previous Surgery | Some patients may have previously undergone knee surgeries (e.g., arthroscopy or partial knee replacement) that did not yield satisfactory results. When pain and dysfunction persist, a total knee replacement may be warranted. |
Additional Factors Considered
While the primary symptoms and conditions are critical in determining the need for a total knee replacement procedure, several additional factors will guide both the patient and physician towards the decision:
- Severity of Symptoms: Surgeons commonly evaluate the intensity and frequency of knee pain, especially the impact on daily activities and overall quality of life.
- Conservative Treatments: Prior to considering surgery, patients often undergo non-surgical treatments like physical therapy, medications, and lifestyle modifications. If these options prove ineffective, surgical options may be considered.
- Patient’s Age and Activity Level: The ideal candidates for knee replacement typically fall within a specific age range—often between 50 and 80 years. Young patients may also be considered if their lifestyle necessitates improved knee function, but their activity levels and prior joint condition will be considered.
- Overall Health: The patient’s general health status is also crucial. Surgeons assess the risk of complications based on pre-existing health conditions such as diabetes, obesity, or cardiovascular diseases.
When to Consider Surgery
Recognizing when to pursue surgical intervention can be challenging. Here are some signs that may indicate the need for a total knee replacement:
- Persistent knee pain that adversely affects daily life.
- Reduced mobility or difficulty walking, standing, or climbing stairs.
- Stiffness that limits movement, particularly after prolonged inactivity.
- Swelling in the knee joint that does not resolve with rest or elevation.
- The reliance on assistive devices (e.g., canes or walkers) for mobility.
In summary, the indications for a total knee replacement are multifaceted, encompassing both damage to the knee joint and diminished quality of life. By carefully assessing the patient’s specific circumstances, orthopedic surgeons can make informed recommendations where surgery becomes necessary to restore function and alleviate pain.
The Pre-Operative Assessment
Preparing for a total knee replacement procedure requires careful planning and thorough evaluation. The pre-operative assessment is a critical step that helps ensure that both the patient and the surgical team are well-prepared for the upcoming surgery. This assessment typically takes place several weeks before the date of the surgery and includes a comprehensive review of the patient’s medical history, physical examination, and various diagnostic tests.
Medical History Review
During the pre-operative assessment, the healthcare provider will start by collecting a detailed medical history. This process involves asking questions about:
- Past surgeries: Any history of previous knee surgeries or other orthopedic procedures.
- Chronic conditions: Existing conditions like diabetes, heart disease, or arthritis which could affect the surgery.
- Medication use: Any prescription or over-the-counter medications, supplements, and blood thinners that may need to be adjusted prior to surgery.
- Allergies: Noting any allergies to anesthesia, medications, or materials typically used in surgery.
Physical Examination
Following the medical history review, a thorough physical examination will take place. This examination aims at assessing the:
- Range of motion: Evaluating how well the knee functions during movement.
- Swelling or deformities: Identifying any visible problems that may impact surgery.
- Overall health: Assessing vital signs including blood pressure, heart rate, and respiratory rate to ensure overall fitness for surgery.
Diagnostic Tests
To ensure optimal conditions for the total knee replacement procedure, various diagnostic tests may be performed. These tests help the surgical team understand the patient’s current knee condition and any underlying health issues. Common tests include:
- X-rays: These imaging tests reveal the extent of damage to the knee joint, cartilage condition, and alignment issues.
- MRI or CT scans: For more detailed images, these advanced imaging techniques help in assessing the soft tissues around the knee.
- Laboratory tests: Blood tests can screen for anemia, electrolyte levels, and kidney function to ensure that the body is prepared for surgery.
Risk Assessment
A significant part of the pre-operative assessment is evaluating the risks associated with the total knee replacement procedure. This typically includes encountering factors like:
- Infection risk: Discussing signs of infection and preventative measures.
- Blood clots: Understanding individual risk factors for thrombosis and strategies to minimize this risk post-surgery.
- Anesthesia risks: Reviewing the types of anesthesia feasible for the patient, especially if they have previous reactions.
Patient Education
Educating the patient about the upcoming surgery is crucial. The healthcare provider will discuss the pre-operative processes, what to expect during the recovery period, and the importance of following pre-surgical instructions. This can include:
- Dietary restrictions: Guidelines for what to eat or avoid as the surgery date approaches.
- Medication modifications: Directions on which medications to continue or discontinue prior to surgery.
- Preparations at home: Suggestions for making the home environment safe and comfortable for recovery, including arranging for assistance with daily tasks.
Summary
The pre-operative assessment serves as a comprehensive evaluation process that ensures patients are well-informed and medically prepared for their total knee replacement procedure. By taking into consideration the patient’s medical history, physical condition, potential risks, and providing education, this assessment plays a vital role in setting the stage for a successful surgical experience and recovery.
Preparing for Surgery: What to Do
Preparing for your total knee replacement procedure is a crucial step that greatly influences your surgical outcome and recovery. Adequate preparation can alleviate anxiety, ensure a smooth process, and enhance post-operative recovery. Here are several essential steps and guidelines to follow in the lead-up to your surgery.
1. Consultation with Your Surgeon
Before the surgery, you’ll have a thorough consultation with your orthopedic surgeon. It’s important to discuss:
- Medical History: Share any pre-existing conditions, medications, and surgeries you’ve had.
- Surgical Technique: Understand the type of knee replacement you’re having (partial vs. total) and the approach (traditional vs. minimally invasive).
- Expected Outcomes: Gain insight into what you can realistically expect post-surgery.
2. Pre-Operative Testing
Your physician may recommend specific tests to ensure you are fit for surgery. These may include:
| Test | Purpose |
|---|---|
| Blood Tests | Check for anemia and organ function |
| Imaging Studies | Assess the severity of knee damage |
| EKG | Evaluate heart health |
| Urinalysis | Rule out infection risks |
3. Medications Review
Prior to surgery, you will need to review your current medications with your healthcare provider. Pay special attention to the following:
- Blood Thinners: These may need to be stopped leading up to your surgery to reduce bleeding risk.
- Over-the-Counter Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) should be discussed, as they may affect your surgical outcome.
4. Lifestyle Adjustments
Certain lifestyle changes can significantly improve your overall health and recovery. Consider incorporating the following:
- Diet: Adopt a balanced diet rich in protein, vitamins, and minerals to support healing.
- Exercise: Engage in low-impact physical activity, as advised by your physician, to strengthen your leg muscles.
- Smoking Cessation: Quitting smoking can reduce complications and accelerate recovery. Seek resources or support if needed.
5. Home Preparation
Prepare your home to facilitate recovery post-surgery:
- Clear Pathways: Ensure your living environment is free from tripping hazards.
- Accessibility: Arrange furniture and commonly used items within easy reach.
- Assistive Devices: Stock up on necessary aids such as crutches, walkers, or raised toilet seats.
6. Plan for Support
Post-surgery, it’s vital to have a support system in place. Coordinate help from family members or friends:
- Transportation: Arrange to have someone drive you to and from the hospital.
- Post-Operative Care: Set up a point of contact for the first few days after surgery for assistance with daily activities.
7. Day Before Surgery Instructions
The day before your total knee replacement procedure is often filled with specific instructions:
- Dietary Restrictions: Follow your surgeon’s advice about food and drink intake prior to your surgery.
- Hygiene: You may be instructed to bathe using an antiseptic soap to minimize infection risks.
- Avoid Makeup or Jewelry: Ensure you come to the hospital free of these items for safety.
By taking these steps, you can set the stage for a successful surgical experience and smoother recovery. Preparedness not only enhances your physical readiness but also instills confidence in navigating this significant life event.
The Day of the Procedure: Step-by-Step
The day of your total knee replacement procedure marks a significant milestone in your journey toward relief from knee pain and improved mobility. Understanding what to expect can alleviate anxiety and help you feel more prepared. Here, we walk you through each step of the day, ensuring you’re fully informed and ready for the procedure.
Arrival at the Hospital
- Check-In: Arrive at the hospital or surgical center at the time designated by your healthcare team. This typically occurs several hours prior to your scheduled surgery. Ensure you have all necessary paperwork and identification, as these will be required during the check-in process.
- Preoperative Assessment: Upon checking in, you will undergo a preoperative assessment. This includes verifying your medical history, discussing any medications, and confirming your understanding of the surgery. You’ll also meet your surgical team, including the anesthesiologist and the orthopedic surgeon.
Preoperative Preparation
- Fasting: You may be instructed not to eat or drink for a specific amount of time before the procedure—often overnight. This ensures your stomach is empty during anesthesia administration, reducing the risk of complications.
- Changing into Surgical Attire: After the assessment, you’ll change into a hospital gown. You’ll also remove any jewelry, contacts, or makeup, which can interfere with the procedure or safety.
Anesthesia Administration
- Anesthesia Options Discussion: Your anesthesiologist will discuss your options for anesthesia, including general anesthesia and regional blocks like spinal or epidural anesthesia. Depending on your overall health and the specifics of your procedure, they will recommend the most appropriate option.
- Receiving Anesthesia: Once you’re ready for surgery, the anesthetic will be administered. You will likely feel a combination of relaxation and drowsiness as the medication takes effect.
Surgical Procedure
- Entering the Operating Room: After anesthesia is administered, you will be transported to the operating room. The surgical team will position you comfortably on the operating table, ensuring that you are safe and secure throughout the procedure.
- Surgical Steps: Your surgeon will perform the total knee replacement procedure, which typically involves the following:
- Removing the damaged cartilage and bone from the knee joint
- Shaping the bone to accommodate the artificial implant
- Inserting the implant and ensuring it fits properly
- Closing the incision with sutures or staples
Post-Anesthesia Recovery
- Post-Anesthesia Care Unit (PACU): After the surgery is completed, you will be transferred to the PACU for monitoring. Healthcare professionals will check your vitals and manage any immediate post-operative pain.
- Family Contact: A healthcare provider will inform your family about the surgery’s outcome and discuss the next steps in your recovery plan.
Summary of the Process
To give you a clearer picture, here’s a quick table summarizing what happens on the day of the procedure:
| Event | Description |
|---|---|
| Arrival | Check-in and initial assessments |
| Preoperative Assessment | Medical history verification and team introductions |
| Fasting | Cease food and drink for safety |
| Changing Attire | Change into a hospital gown and remove personal items |
| Anesthesia Discussion | Talk about anesthesia options and health considerations |
| Receiving Anesthesia | Administering anesthesia for comfort during surgery |
| Surgery | Performing the total knee replacement procedure |
| Recovery | Monitoring in PACU and pain management |
Understanding the day of the procedure can lighten the emotional load leading up to surgery. Knowing what to expect helps prepare you for each phase, paving the way for a smoother transition into recovery.
Understanding Anesthesia Options
When undergoing a total knee replacement procedure, one crucial aspect that patients should understand is the type of anesthesia that will be administered during the surgery. Anesthesia not only alleviates pain but also ensures that patients remain relaxed and comfortable throughout the operation. In this section, we will explore the various anesthesia options available, the benefits and risks associated with each type, and factors influencing the decision process.
Types of Anesthesia
There are primarily three types of anesthesia used in surgical procedures, including total knee replacements:
- General Anesthesia
General anesthesia renders patients completely unconscious. It involves the administration of anesthetic drugs intravenously and/or inhaled gases. This choice is often utilized for patients who may be apprehensive or for those undergoing longer or more complex procedures. However, a potential drawback includes the longer recovery period, where patients might experience grogginess or confusion upon waking. - Regional Anesthesia
Regional anesthesia is another popular choice for knee surgeries. This technique blocks pain in a specific area of the body, such as the leg, and can be classified into two main categories:- Spinal Anesthesia: This involves injecting anesthetic into the fluid surrounding the spinal cord, effectively numbing the lower half of the body. Patients usually remain awake but are free from sensations in their legs and lower abdomen.
- Epidural Anesthesia: Similar to spinal anesthesia, it is administered through a catheter placed in the epidural space, allowing for continuous pain relief throughout and after the surgery.
The benefits of regional anesthesia include a faster recovery from anesthesia, reduced pain levels post-surgery, and a decreased need for opioid pain medications.
- Local Anesthesia
Local anesthesia is the least commonly used option for total knee replacement procedures, as it involves numbing only a small area. It is typically reserved for minor procedures, not suitable for a major surgery like a total knee replacement, as it may not provide sufficient pain relief for the surgery duration.
Factors Influencing Anesthesia Choice
The decision of which anesthesia to use is personalized and can depend on various factors, including:
- Patient Health: Pre-existing medical conditions, medications, and overall health can influence the choice of anesthesia.
- Duration and Complexity of Surgery: Longer and more complex surgeries may necessitate general anesthesia for complete pain control and patient comfort.
- Patient Preference: In some cases, patients may express a preference for one type of anesthesia over another based on previous experiences or fears.
Risks and Considerations
Each anesthesia type carries inherent risks.
- General Anesthesia Risks: Potential complications include allergic reactions, respiratory issues, and lingering effects like nausea or confusion.
- Regional Anesthesia Risks: These may include headaches, temporary weakness, nerve injury, or infection at the injection site.
It is essential to have a thorough discussion with your anesthesiology team, who will evaluate your individual case and guide you toward the safest and most appropriate option for your total knee replacement procedure.
In Summary
Understanding the anesthesia options available for a total knee replacement procedure is vital for patients to make informed decisions alongside their healthcare providers. Weighing the benefits against the potential risks, in conjunction with individual health considerations, will help ensure a smooth surgery and recovery process. By being well-informed, patients can approach their surgery with confidence, knowing they have selected the most suitable anesthesia method for their needs.
Post-Operative Care and Recovery
The post-operative care and recovery phase following a total knee replacement procedure is critical to the overall success of the surgery. This phase not only ensures a smooth transition back to daily activities but also plays a significant role in enhancing rehabilitation and long-term outcomes. Proper attention to care can greatly influence the healing process, make pain management easier, and help avoid complications.
Initial Post-Operative Care
Immediately after the surgery, the patient will be moved to a recovery room where medical staff will monitor vital signs such as heart rate, blood pressure, and oxygen levels. It’s important to have a responsible adult accompany you to the hospital, as you will likely be advised not to drive for several weeks following the procedure.
During the first 24 hours, your care may involve:
| Care Aspect | Description |
|---|---|
| Monitoring Vital Signs | Nurses will check your heart rate, blood pressure, and oxygen saturation regularly. |
| Pain Management | Pain relief medications will be administered to minimize discomfort. |
| Fluid and Nutrition Intake | Initially, you may receive fluids through an IV; solid foods will gradually be introduced based on your tolerance. |
| Infection Prevention | Antibiotics may be given to prevent infection. Wounds will also be monitored closely. |
Returning Home
Once stable, patients are typically discharged within one to three days post-surgery, depending on individual circumstances and the surgical facility’s protocols. Prior to going home, ensure you have made the necessary arrangements for assistance, as mobility will be limited during the initial phase of recovery. Here are some essential tips to consider when preparing for discharge:
- Home Modifications: Remove tripping hazards, secure loose rugs, and establish a clear path to your bathroom and bedroom.
- Assistive Devices: Acquire crutches or a walker if prescribed, as they will be crucial for mobility during the early recovery period.
- Follow-Up Appointments: Schedule any necessary follow-up consultations with your healthcare provider to ensure proper healing and monitor progress.
Rehabilitation Process
The rehabilitation process typically begins within the first 48 hours after surgery. Engaging in physical therapy is vital to regain strength and restore function in the knee joint. Here’s what you can generally expect:
| Rehabilitation Stage | Focus | Goals |
|---|---|---|
| Phase 1: Early Mobility | Gentle range-of-motion exercises | Reduce stiffness and swelling |
| Phase 2: Strengthening | Targeted strength-building exercises | Improve muscle function |
| Phase 3: Return to Activity | Gradual reintegration of daily activities | Achieve normal mobility |
Post-operative care also emphasizes regular monitoring for symptoms such as increased pain, swelling, redness, or fever, which could indicate complications. It’s imperative to keep the surgical area clean and dry, avoid soaking it in water until cleared by your doctor, and follow any specific instructions regarding wound care.
Long-Term Recovery and Outcomes
Initially, it may take up to six weeks for the knee to heal adequately, but complete recovery can last several months. Most patients notice significant improvement in pain relief and function within three to six months following the total knee replacement procedure. Regular follow-ups with your surgeon and persistent adherence to rehabilitation protocols are key to achieving optimal results.
Understanding these aspects of post-operative care and recovery helps set realistic expectations, fosters proactive engagement with rehabilitation, and ultimately contributes to a successful return to an active lifestyle.

Managing Pain After Surgery
Recovery following a total knee replacement procedure typically involves a regimented approach to pain management. Understanding the different pain management strategies can significantly enhance your recovery experience. Here, we explore several effective methods to manage pain post-surgery, ensuring your comfort as you embark on the journey of rehabilitation.
Immediate Post-Operative Pain Management
Upon waking in the recovery room, patients often receive a combination of medications tailored to control pain as effectively as possible. Some common options include:
| Medication Type | Purpose | Notes |
|---|---|---|
| Opioids | To relieve moderate to severe pain | Used in the short term for best results |
| Non-steroidal anti-inflammatory drugs (NSAIDs) | To reduce inflammation and mild pain | Over-the-counter options may be available |
| Acetaminophen | For mild pain relief | Often used in conjunction with NSAIDs |
An individualized pain management plan is typically devised by your healthcare team to address your specific needs.
Outpatient Pain Management Strategies
As patients transition from the hospital to home, they can employ various strategies to continue managing pain effectively:
- Medications: Continue taking prescribed pain relief medications as directed. Be mindful of the timings for optimal relief.
- Ice Therapy: Applying ice packs to the surgical area can help reduce swelling and numb the area, providing temporary relief. Always use a cloth barrier to protect the skin.
- Elevation: Keeping the knee elevated above the level of the heart can significantly decrease swelling, thereby aiding in pain reduction.
- Rest: Allocate sufficient time for rest. Avoid overexertion to prevent unnecessary strain and discomfort.
Complementary Therapies
Incorporating complementary treatments can also enhance pain management. Patients might consider:
- Physical Modalities: Utilizing heat or cold packs can alleviate discomfort. A heating pad may also help soothe the muscles around the knee post-inflammation.
- Massage Therapy: Gentle massage around the surgical area once cleared by a doctor can provide relief and improve blood circulation.
- Mindfulness Techniques: Practices such as deep breathing, meditation, or guided imagery may aid in reducing the perception of pain.
Progress Monitoring and Communication
It’s essential to maintain open communication with your healthcare team about pain levels. They may adjust medications or suggest alternative methods if pain management is insufficient. Also, keep a pain diary to track your pain intensity and response to treatments; this will be invaluable for discussions with your healthcare providers.
Understanding Pain Expectations
Pain should gradually improve over time after surgery. However, it is essential to recognize that the first few weeks post-surgery may involve varying levels of discomfort.
- First 1-2 Weeks: Moderate to severe pain that typically peaks in the first week.
- Weeks 2-4: Pain starts to decrease; many patients begin to transition off opioids.
- 1 Month and Beyond: Most patients experience considerable improvement, moving towards minor discomfort that can be managed with NSAIDs or acetaminophen.
By following these comprehensive pain management strategies, you can create a more tolerable and effective recovery experience after your total knee replacement procedure. Always consult with your healthcare providers before starting or altering any pain management regimen.
Physical Therapy and Rehabilitation
The journey towards a full recovery following a total knee replacement procedure is heavily reliant on structured physical therapy and rehabilitation. This phase is essential not only for regaining physical strength but also for enhancing mobility and ensuring successful outcomes in the long run. Let’s explore the critical components of physical therapy and rehabilitation, focusing on their phases, benefits, and effective management strategies.
Importance of Physical Therapy
After undergoing a total knee replacement procedure, patients typically face challenges concerning mobility, strength, and function. Physical therapy plays a fundamental role in addressing these challenges by:
- Restoring Range of Motion: An essential goal post-surgery, physical therapy focuses on minimizing stiffness in the knee joint. Therapists design specific exercises aimed at gradually increasing flexibility.
- Enhancing Muscle Strength: Strengthening the muscles around the knee provides stability and support to the newly operated joint. Focus is placed on quadriceps, hamstrings, and calf muscles.
- Promoting Functional Independence: As patients progress, activities of daily living, such as walking, climbing stairs, and getting in and out of a chair, become key focuses.
Rehabilitation Timeline
The rehabilitation process typically unfolds in a series of stages. Below is a general timeline for recovery post-surgery:
| Rehabilitation Phase | Timeframe | Goals |
|---|---|---|
| Phase 1: Initial Recovery | Weeks 1-2 | Control swelling, regain passive range of motion, and begin gentle active exercises. |
| Phase 2: Early Rehabilitation | Weeks 3-6 | Increase active range of motion, build strength, and start basic functional activities. |
| Phase 3: Advanced Rehabilitation | Weeks 6-12 | Focus on improving strength, balance, and mobility through more dynamic exercises. |
| Phase 4: Return to Activity | 3 months and beyond | Gradually resume normal activities and sports; continue to build muscle strength and stability. |
Components of Physical Therapy
During physical therapy sessions, you may engage in a variety of exercises and techniques, including:
- Therapeutic Exercises: Customized exercise routines focusing on strengthening and flexibility.
- Manual Therapy Techniques: Hands-on therapy applied by the therapist, addressing joint stiffness and muscle tightness.
- Gait Training: Learning how to walk correctly with assistive devices initially, gradually working towards walking independently.
Patient-Centered Approach
Each rehabilitation plan should be uniquely tailored to the individual, taking into account:
- Patient’s Pre-Surgery Fitness Level: Those accustomed to regular activity may have different starting points compared to less active individuals.
- Comorbidities: Pre-existing health conditions can influence rehabilitation. Strategies must accommodate these factors for effective recovery.
- Patient Goals and Lifestyle: Understanding what patients wish to achieve post-rehabilitation guides tailored exercise and activity plans.
Monitoring Progress
Throughout the rehabilitation process, monitoring progress is crucial. Physical therapists regularly assess:
- Range of Motion: Tracking the flexibility of the knee to establish movement improvements.
- Strength Levels: Measuring gains in muscle strength to ensure progression.
- Pain Levels: Addressing any discomfort or pain that may arise during physical activities.
By the end of the rehabilitation process, patients should expect significant improvements in their mobility and strength, setting the stage for a fulfilling lifestyle after the total knee replacement procedure. Proper adherence to prescribed therapy plans and active participation in recovery can greatly influence long-term results.
Long-Term Outcomes and Expectations
When considering a total knee replacement procedure, it is crucial to understand the long-term outcomes and expectations post-surgery. The primary goal of this surgery is to improve the quality of life by alleviating pain, restoring function, and enhancing mobility. However, the results can vary based on several factors, including the patient’s age, overall health, and adherence to rehabilitation protocols.
Key Long-Term Outcomes
- Pain Relief
- One of the most significant benefits reported by patients is substantial pain relief. Studies show that approximately 90% of individuals experience reduced pain levels within the first year after the procedure.
- Improved Mobility
- Patients generally see improved mobility, enabling them to participate in daily activities and exercise more comfortably. This enhancement often leads to a greater sense of independence.
- Functionality Improvements
- The overall knee function is markedly enhanced, allowing patients to engage in activities like walking, climbing stairs, and participating in sports with minimal discomfort.
- Longevity of the Implant
- Modern implants are designed to last 15 to 25 years under normal conditions. Regular follow-ups with healthcare providers can help ensure the implant remains in good condition.
- Quality of Life
- Many patients experience a remarkable boost in their overall quality of life, as they can return to hobbies and activities previously hindered by knee pain.
Factors Affecting Long-Term Success
Certain factors can significantly influence the long-term success of the procedure. Consider the following:
| Factor | Impact on Outcome |
|---|---|
| Patient Age | Younger patients often have better outcomes due to greater healing capacities. |
| Weight Management | Maintaining a healthy weight reduces stress on the knee and improves implant longevity. |
| Comorbidity | Conditions such as diabetes or cardiovascular disease can complicate recovery and outcomes. |
| Adherence to Rehabilitation | Engaging in prescribed physical therapy enhances recovery and overall success. |
| Lifestyle Choices | Smoking and poor nutrition can hinder the healing process. |
Expectations for Recovery
Understanding what to expect during recovery is vital for setting realistic goals. Initially, post-operative pain management will be intensive, but as healing progresses, pain levels will reduce significantly. Patients can typically expect:
- Weeks 1-2: Focus on pain management and basic mobility (walking with assistance).
- Weeks 3-6: Increased physical therapy sessions focusing on strength and mobility exercises.
- Months 2-3: Most patients are able to resume light activities. Daily routines can often return to normal during this period.
- Months 6-12: Full recovery is typically achieved, with most patients returning to pre-surgery activity levels.
After the initial recovery phase, most patients will find that their knees feel better than they have in years. Regular follow-up appointments with your surgeon will help monitor the condition of the knee and discuss any concerns you may have.
In summary, while the total knee replacement procedure offers promising long-term outcomes and the potential for a significantly improved quality of life, it is essential for patients to commit to their rehabilitation and follow up with health care providers to ensure the best possible results. Understanding and preparing for these expectations can greatly enhance the recovery experience period and overall satisfaction with the surgery.
Frequently Asked Questions
What is a total knee replacement procedure?
A total knee replacement procedure, also known as total knee arthroplasty, is a surgical operation where a damaged or diseased knee joint is replaced with artificial components. This procedure is typically recommended for individuals suffering from severe knee pain or disability due to conditions like arthritis. The surgery aims to restore joint function, improve mobility, and reduce pain, allowing patients to return to daily activities more comfortably.
What should I expect during the initial consultation?
During the initial consultation for a total knee replacement procedure, the orthopedic surgeon will perform a comprehensive evaluation. This includes reviewing your medical history, discussing your symptoms, and conducting a physical examination. Imaging tests such as X-rays or MRIs may also be ordered to assess the extent of damage to your knee joint. Based on these assessments, the surgeon will explain the procedure, potential risks, and expected outcomes, helping you make an informed decision.
What is the recovery process like after surgery?
The recovery process following a total knee replacement typically involves several stages. Immediately after surgery, patients are encouraged to begin gentle movements to promote blood circulation. Rehabilitation usually starts within the first few days, focusing on physical therapy that strengthens the knee and improves flexibility. Full recovery can take several months, but most patients can expect to return to normal activities, including walking and light exercise, within six to twelve weeks if they adhere to the rehab plan.
What are the potential risks and complications associated with the procedure?
As with any surgical procedure, total knee replacement comes with potential risks and complications. These may include infections, blood clots, nerve damage, implant failure, or persistent pain. Moreover, some patients may experience stiffness or limited range of motion post-surgery. However, these risks can be minimized through proper surgical techniques, adherence to post-operative care, and engaging in physical therapy as recommended by healthcare providers.
How long do knee implants typically last?
Knee implants are designed to be durable and can last for many years. On average, most knee replacements last anywhere from 15 to 20 years, depending on various factors, including the patient’s age, activity level, and overall health. While replacement parts may wear out over time, newer prosthetics and advanced surgical techniques are leading to longer-lasting results. Regular follow-ups with your orthopedic surgeon can help monitor the condition of the implant.